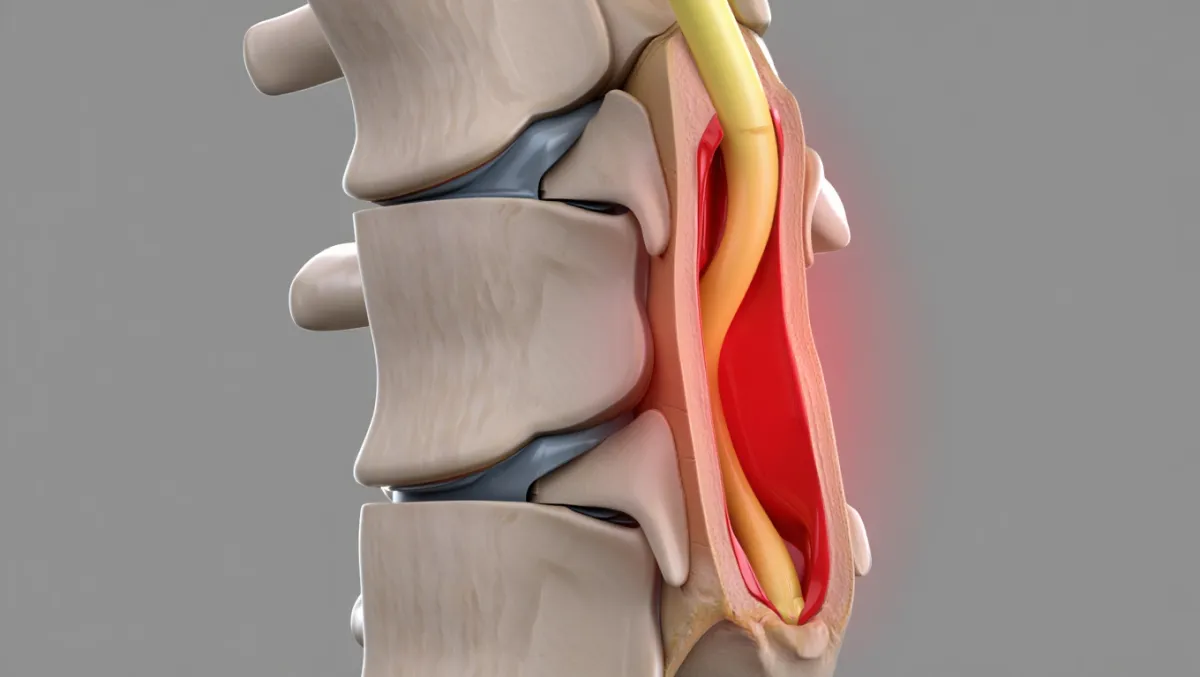
Stenosis
Thoracic Stenosis Surgery
Relieving Pressure in the Mid-Back to Protect the Spinal Cord
Thoracic spinal stenosis occurs when the spinal canal in the mid-back narrows, compressing the spinal cord or nerve roots. Though less common than lumbar or cervical stenosis, it can cause mid-back pain, numbness, weakness, balance problems, or even paralysis if left untreated. At Desert Spine and Pain, neurosurgeon Dr. David L. Greenwald, M.D., FAANS, FACS provides expert surgical care for thoracic stenosis, using microsurgical and minimally invasive techniques whenever possible. Our goal is to relieve compression, protect the spinal cord, and restore your function and confidence.

Over 100 5-Star Reviews!


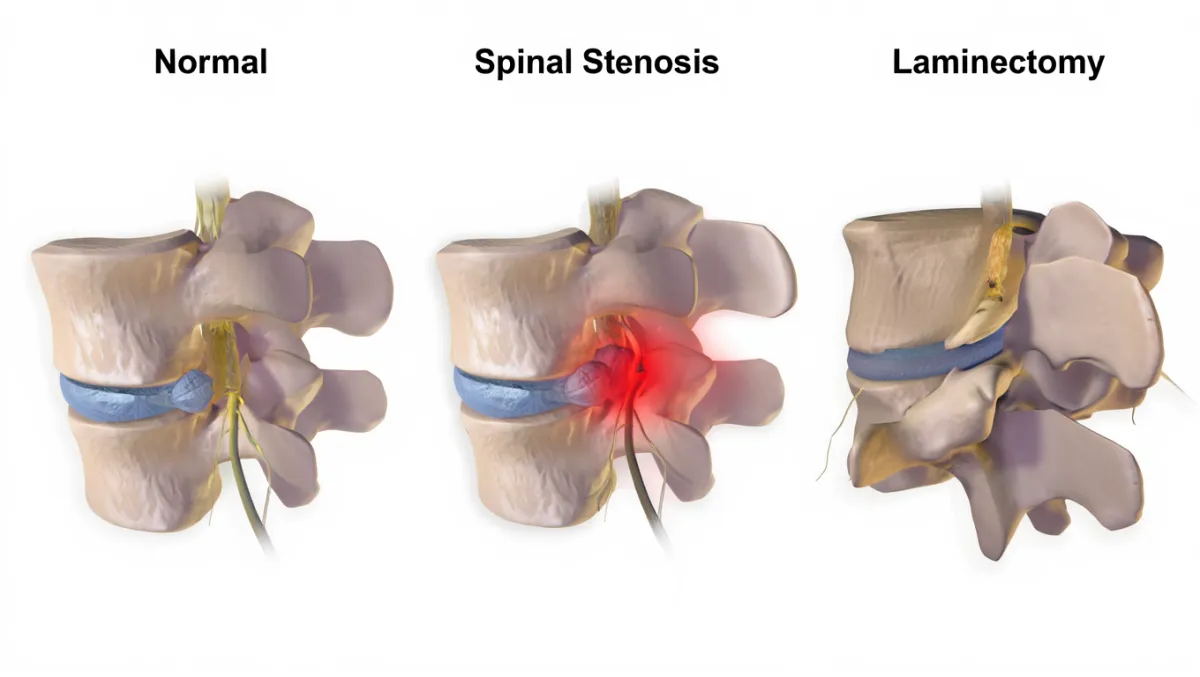
What Is Thoracic Stenosis Surgery?
In simple terms: The surgery removes bone, ligament, or disc material pressing on the spinal cord in the thoracic spine (mid-back), creating more room.
Scientifically: Thoracic stenosis decompression may involve laminectomy, laminotomy, foraminotomy, or discectomy, with or without fusion, to enlarge the spinal canal and relieve cord/nerve compression. Microsurgical and image-guided techniques are often used due to the tight canal and high stakes in the thoracic spine.

Conditions Treated
Thoracic spinal stenosis (degenerative or congenital)
Thoracic disc herniation
Myelopathy from cord compression
Radiculopathy (thoracic nerve root pain, numbness, or weakness)
Stenosis from ossification of the ligamentum flavum (OLF) or ossification of the posterior longitudinal ligament (OPLL)
Post-traumatic stenosis or deformity
Types of Thoracic Stenosis Surgery
1. Thoracic Laminectomy
Removes the lamina to decompress the spinal cord.
Used for multi-level stenosis.
2. Thoracic Laminotomy / Foraminotomy
Removes part of the lamina or widens the foramen to relieve nerve root compression.
Often performed minimally invasively.
3. Thoracic Discectomy
Removal of herniated disc compressing the spinal cord or nerves.
May require an anterior, lateral, or posterolateral approach depending on location.
4. Thoracic Fusion (when needed)
Added if instability is present or created during decompression.
Uses bone graft and screws/rods to stabilize the spine.

The Thoracic Stenosis Procedure: Step by Step
Plain-English Overview
Anesthesia & positioning: You’re asleep under general anesthesia.
Incision: A small incision is made in the mid-back (posterior approach most common).
Decompression: Bone, ligament, or disc material pressing on the cord is carefully removed.
Stabilization (if needed): Screws and rods may be added to prevent instability.
Closure: The incision is closed; recovery begins the same or next day.
Surgeon-Level Detail
Approach: Posterior midline incision for laminectomy/laminotomy; lateral thoracotomy or MIS lateral access for disc herniations.
Decompression: High-speed drill and Kerrisons used for lamina removal; ligamentum flavum or ossified ligament carefully resected; disc fragments excised under microscope.
Fusion decision: Based on facet removal, deformity, or instability; pedicle screws/rods inserted if required.
Closure: Meticulous hemostasis; layered closure; drain use varies.
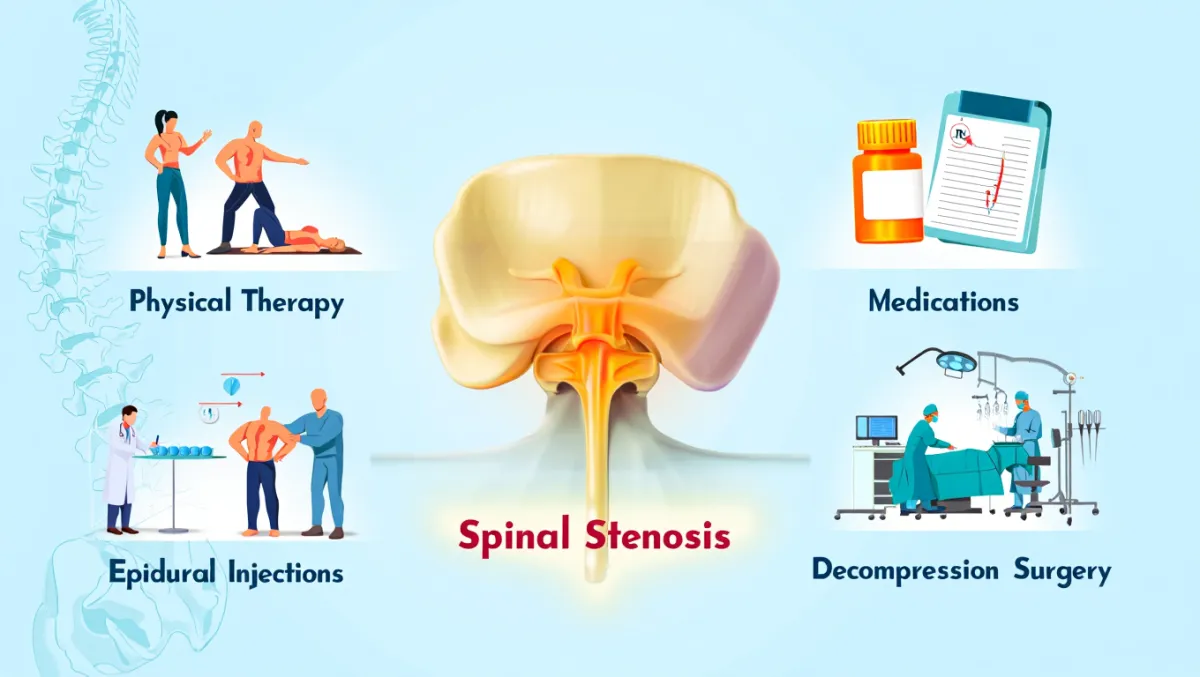
Benefits of Thoracic Stenosis Surgery
Protects the spinal cord from further damage
Relieves mid-back pain, numbness, and weakness
Improves walking tolerance and balance
Prevents progression to paralysis in severe cases
Minimally invasive options available in select cases
Risks & Limitations
Thoracic spine surgery carries higher risk due to proximity of the spinal cord
Infection, bleeding, dural tear/CSF leak
Neurologic injury (weakness, paralysis—rare with neurosurgical precision)
Instability requiring fusion
Recovery slower than lumbar/cervical surgery in some patients
Recovery Timeline
Day 0–1: Walking begins with assistance; hospital stay 1–3 days typical
Weeks 1–2: Wound care, light walking daily
Weeks 2–6: Gradual activity increase; desk work often resumed
6–12 weeks: Structured physical therapy; improved mobility and confidence
3–6 months: Steady functional recovery; many return to normal activity
6–12 months: Full healing and fusion (if performed) confirmed with imaging
Why Choose Desert Spine and Pain?
Expert neurosurgeon: Dr. Greenwald is highly experienced with complex thoracic decompressions
Advanced tools: Microsurgical, navigation, and minimally invasive approaches for safety
Comprehensive care: Conservative options first, surgery only when needed
Patient-first philosophy: We explain everything clearly to reduce fear and anxiety about surgery
Frequently Asked Questions
How is thoracic stenosis surgery different from lumbar or cervical surgery?
The thoracic canal is narrower and the cord more vulnerable, so surgery requires extreme precision. It’s less common but more delicate.
Will I need a fusion?
Fusion is only added if instability is present or created during decompression. Many thoracic decompressions don’t require fusion.
How soon will I see improvement?
Leg symptoms (weakness, numbness, walking ability) often improve within weeks to months. Recovery is slower if myelopathy has been present for a long time.
What are the risks?
Thoracic stenosis surgery carries higher risks than lumbar or cervical due to anatomy. With neurosurgical precision, outcomes are very good, but patients must understand the seriousness of the procedure.
How does Desert Spine and Pain perform thoracic stenosis surgery differently?
We use microscope-assisted precision, MIS techniques where appropriate, and neurosurgical expertise to maximize safety and recovery.




Dr. David L. Greenwald, MD
Neuro-Spine Surgeon

Call Now!
Desert Spine and Pain
A Spine Specialist is standing by.
Relief is just a phone call away!
Available Around the Clock.
Phone: (602) 566-9500
Email: [email protected]
Contact Us

Book a Consultation.
If you’re experiencing back pain, balance issues, or leg weakness caused by thoracic spinal stenosis, timely treatment is essential. Dr. Greenwald and his caring team will conduct a thorough evaluation, review your imaging, and determine whether Thoracic Stenosis Surgery is the best option for your condition. Every step you take toward expert spine care brings you closer to comfort, mobility, and peace of mind. Schedule your consultation today and learn how Dr. Greenwald’s specialized approach to thoracic spine surgery can help you regain control of your health and quality of life.

Voted Best Spine Doctor
Over 30 Years Experience in Orthopedic & Neuro Spine Surgeries.

Dr. David L. Greenwald, M.D., F.A.C.S.
Neurosurgeon | Spine Surgeon | Regenerative Medicine
Dr. David L. Greenwald, MD, FACS, is a board-certified spine surgeon with advanced expertise in Thoracic Stenosis Surgery, a procedure designed to relieve pressure on the spinal cord or nerves within the mid-back region. Thoracic spinal stenosis occurs when the spinal canal narrows due to bone spurs, disc herniation, or degenerative changes, leading to pain, stiffness, or even weakness in the torso and legs. Dr. Greenwald uses precision-guided imaging and minimally invasive techniques to safely decompress the spinal canal, restore nerve function, and prevent further neurological damage. His extensive surgical experience and patient-focused care help individuals throughout South Florida achieve meaningful pain relief, improved mobility, and better spinal stability.
Book your Spine Care Consultation Today!


Desert Spine and Pain
Patient Centered & Partner Focused
Quick Links
Resources
Connect With Us
© Desert Spine and Pain. 2026. All Rights Reserved. Sitemap