Minimally Invasive Surgery
Microdiscectomy
Precise Removal of Herniated Disc Material
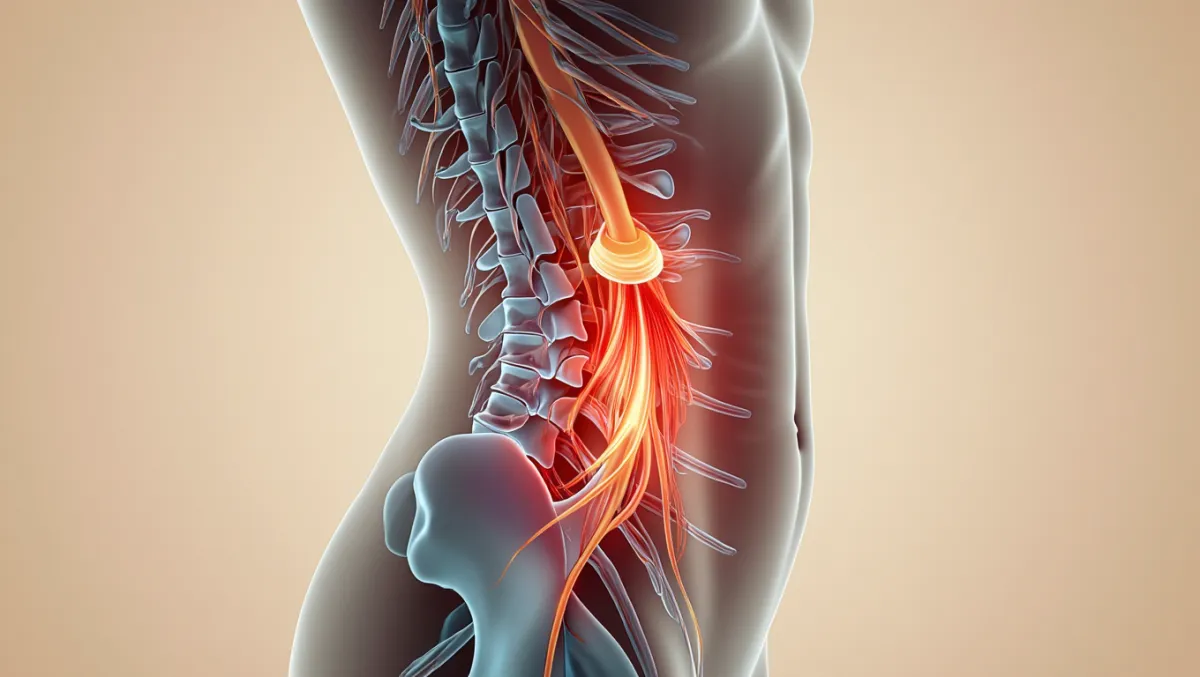
A microdiscectomy is one of the most common minimally invasive spine surgeries. It’s designed to relieve nerve compression caused by a herniated disc, which can trigger sciatica, numbness, tingling, or weakness in the arms or legs. At Desert Spine and Pain, neurosurgeon Dr. David L. Greenwald, M.D., FAANS, FACS specializes in minimally invasive microdiscectomy using small incisions, high-powered microscopes, and microsurgical tools. This means faster recovery, less pain, and highly precise decompression of pinched nerves.

Over 100 5-Star Reviews!

What Is a Microdiscectomy?
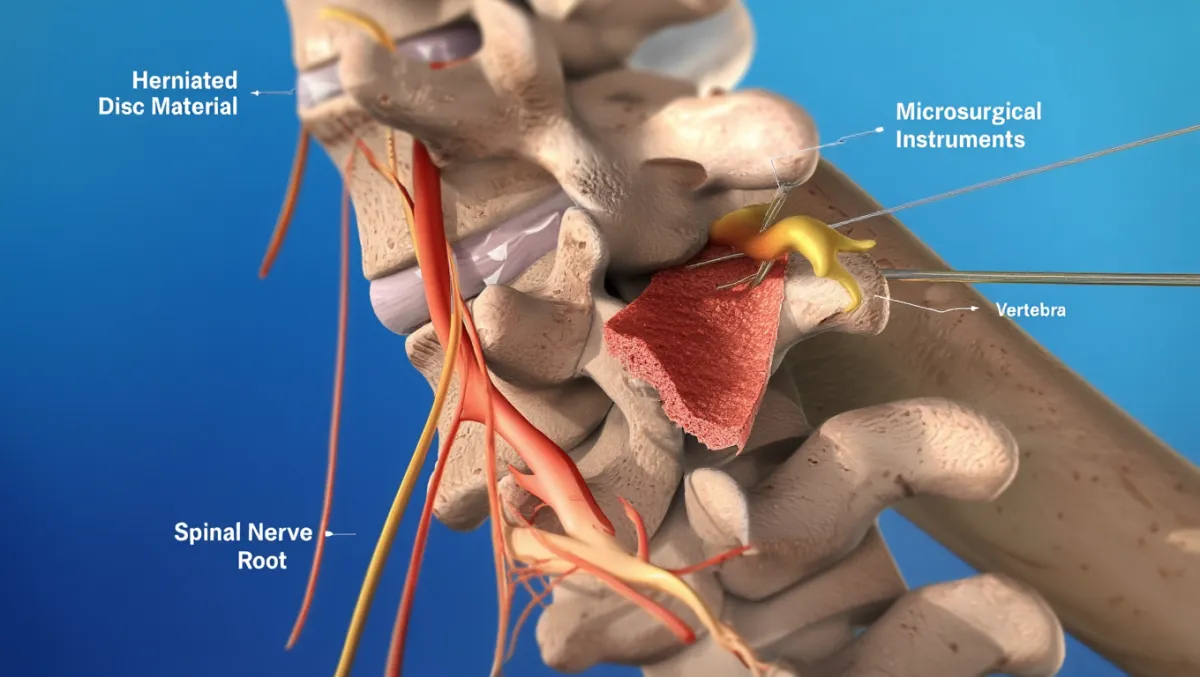
In simple terms: We make a tiny incision in the back, remove the piece of disc that’s pressing on a nerve, and leave the rest of the disc intact.
Scientifically: Microdiscectomy involves laminotomy and flavectomy through a tubular retractor system, followed by removal of herniated nucleus pulposus fragments compressing the traversing/exiting nerve root. The annulus and remaining disc are preserved to maintain stability.
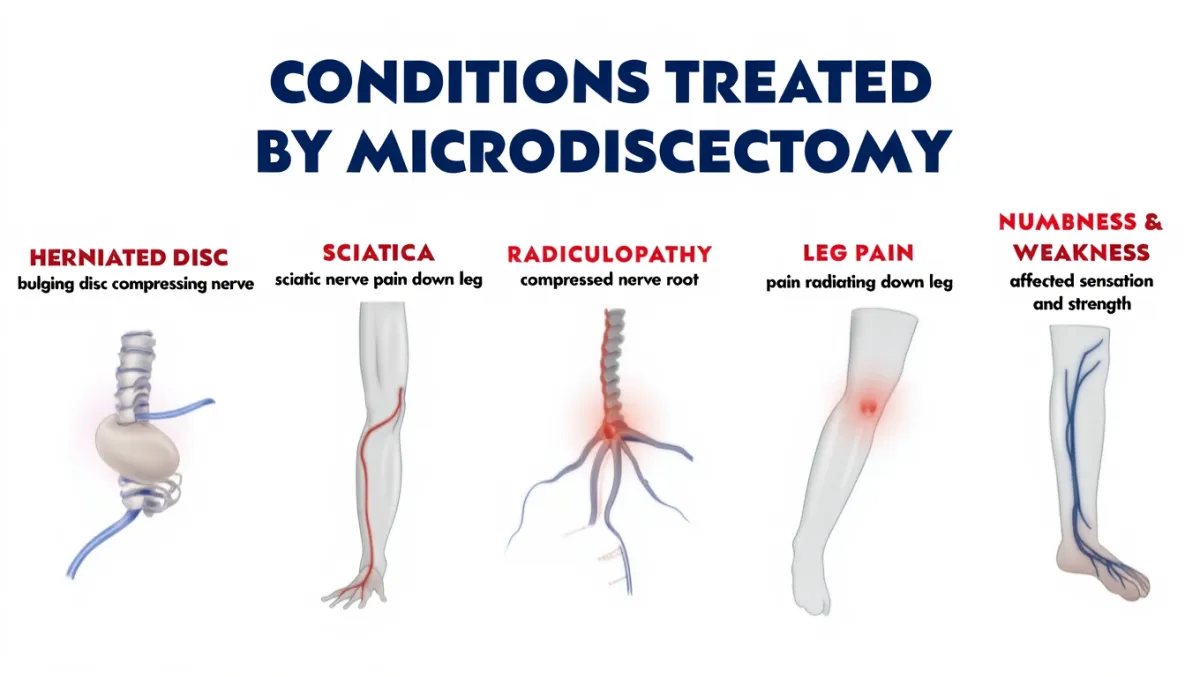
Conditions Treated
Herniated disc with leg or arm pain (sciatica, radiculopathy)
Lumbar radiculopathy (leg pain from compressed spinal nerve)
Cervical radiculopathy (select cases, usually ACDF preferred)
Failed conservative treatment (PT, medications, injections)
Progressive weakness or neurological deficits from nerve compression
Pre-Operative Preparation
Imaging: MRI (gold standard) to identify level and size of herniation; X-rays or CT for bony anatomy if needed
Diagnostics: EMG/NCV may confirm nerve root involvement
Medical clearance: Blood work, anesthesia evaluation, review of medications (especially blood thinners/NSAIDs)
Prehab: Core strengthening and walking programs improve recovery
The Microdiscectomy Procedure: Step by Step
Plain-English Overview
Anesthesia & positioning: You’re asleep under general anesthesia, lying face down.
Small incision: A 1–2 cm incision is made over the affected level.
Muscle-sparing access: A tubular retractor gently spreads muscle fibers apart.
Microscope setup: A surgical microscope provides magnification and lighting.
Partial bone removal: A small window (laminotomy) is made to reach the nerve.
Disc fragment removal: Only the piece pressing on the nerve is removed.
Nerve decompression: The nerve root is gently freed and confirmed to be mobile.
Closure: The incision is closed with sutures or glue.
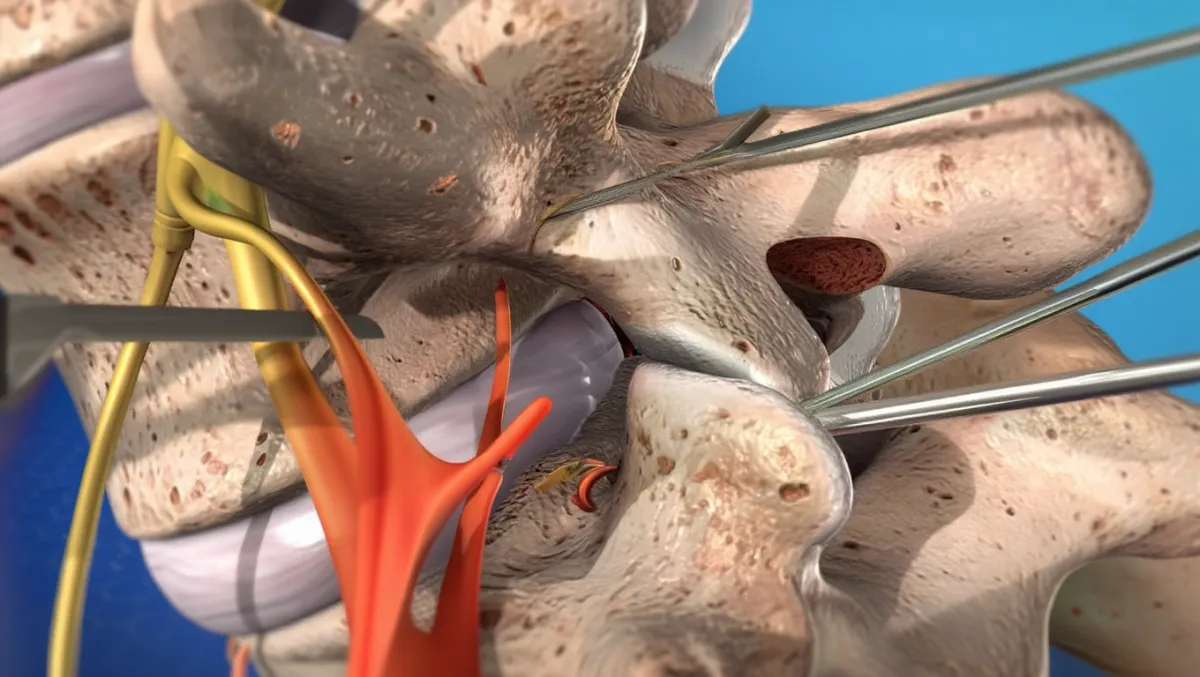
Surgeon-Level Detail
Docking: Fluoroscopy confirms correct level; tubular retractor docked.
Laminotomy & flavectomy: Kerrison punches/drill remove a small portion of lamina and ligamentum flavum.
Nerve visualization: Dural sac and traversing root gently mobilized with microdissectors.
Discectomy: Herniated nucleus fragment(s) identified and removed with pituitary rongeurs; annular defect inspected.
Confirmation: Nerve root inspected for pulsation and free mobility.
Hemostasis & closure: Irrigation, bipolar cautery, retractor removal, layered closure.
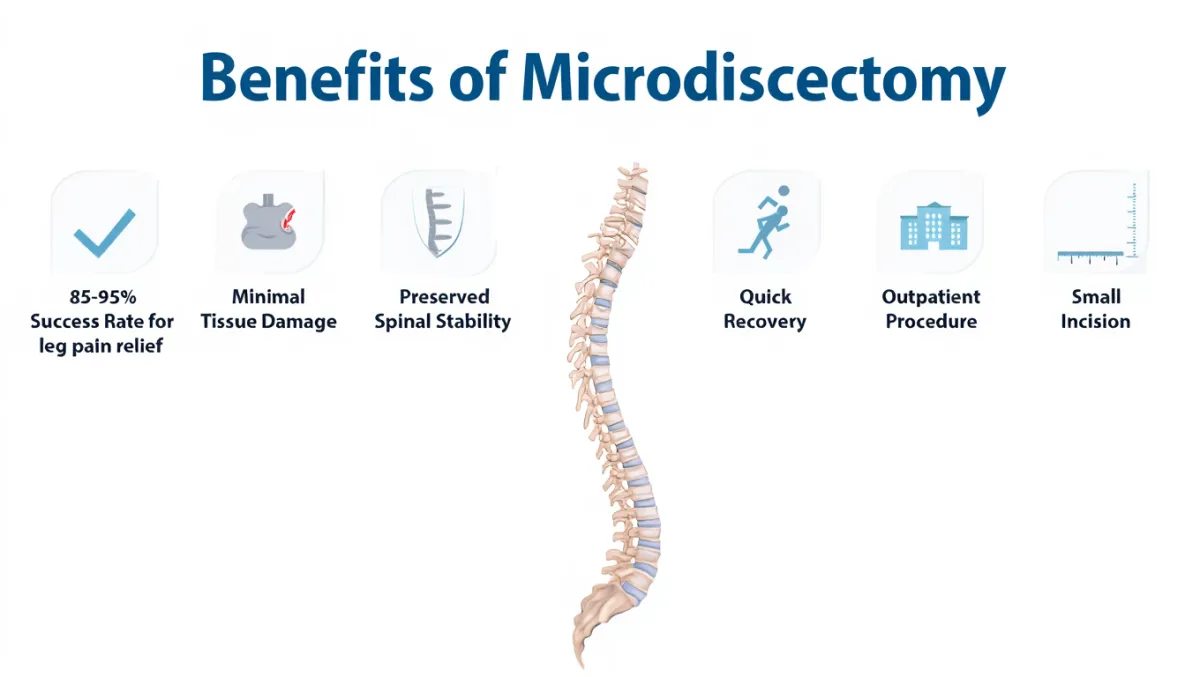
Benefits
Outpatient or 1-night stay
Immediate relief of sciatica in most cases
Tiny incision, minimal scarring
Preserves spinal stability (only fragment removed)
Short recovery time compared to open surgery
Risks & Limitations
Recurrence of disc herniation (5–15% risk)
Infection, bleeding, dural tear/CSF leak
Nerve root irritation or residual numbness
Rare instability if excessive bone removed
Not a cure for back pain alone (best for nerve compression symptoms)
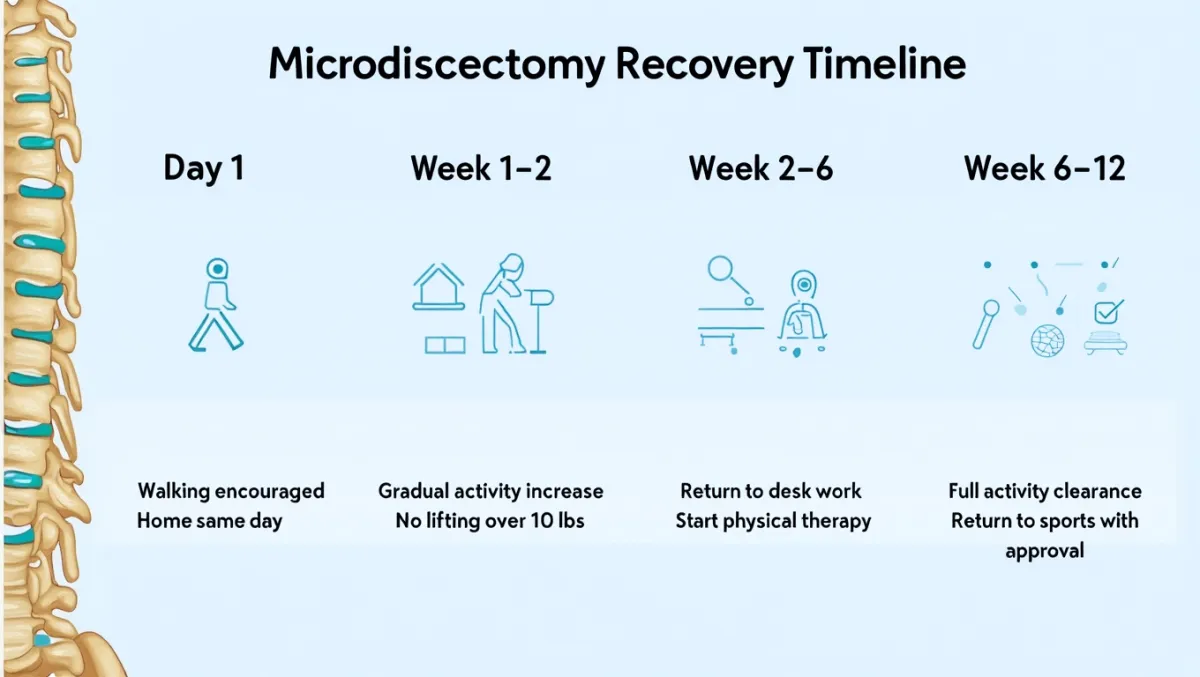
Recovery Timeline
Day 0: Walking within hours; many patients go home the same day
1–2 weeks: Light activities, short walks daily
2–6 weeks: Desk work; avoid bending/lifting/twisting
6–12 weeks: Return to most activities with PT support
3–6 months: Nerve healing continues; strength and sensation improve
Full activity: Typically cleared at 3 months (except high-impact sports, which may take longer)
Why Choose Desert Spine and Pain?
Expert neurosurgeon – Dr. Greenwald is highly experienced in MIS microdiscectomy
Conservative-first approach – Surgery only when injections, PT, and other care fail
Precision tools – Microscopes, tubular retractors, and navigation for accuracy and safety
Compassionate care – We take time to explain every step and guide recovery confidently
Frequently Asked Questions
How do I know if I need a microdiscectomy?
If you have persistent leg or arm pain from a herniated disc that hasn’t improved with conservative care—or if you have progressive weakness—you may be a candidate.
Is recovery painful?
Most patients report immediate relief of leg pain, with manageable incision soreness that improves quickly.
Will the disc re-herniate?
It can in 5–15% of cases. If it does, revision surgery may be needed, or fusion if instability develops.
How soon can I work after surgery?
Desk jobs: 2–4 weeks. Physical jobs: 6–12 weeks depending on activity.
How does Desert Spine and Pain perform microdiscectomy differently?
We use the least invasive approach possible, with Dr. Greenwald’s neurosurgical precision, advanced tools, and a focus on faster recovery.




Dr. David L. Greenwald, MD
Neuro-Spine Surgeon

Call Now!
Desert Spine and Pain
A Spine Specialist is standing by.
Relief is just a phone call away!
Available Around the Clock.
Phone: (602) 566-9500
Email: [email protected]
Contact Us

Schedule a Consultation
If you’re suffering from persistent leg or back pain due to a herniated disc, a microdiscectomy may be the solution you’ve been searching for. Dr. Greenwald and his compassionate team will evaluate your condition and determine if this minimally invasive approach is right for you. Every step you take toward treatment brings you closer to relief, strength, and restored movement. Schedule your consultation today and discover how Dr. Greenwald’s surgical expertise can help you return to a more active, pain-free life.

Voted Best Spine Doctor
Over 30 Years Experience in Orthopedic & Neuro Spine Surgeries.

Dr. David L. Greenwald, M.D., F.A.C.S.
Neurosurgeon | Spine Surgeon | Regenerative Medicine
Dr. David L. Greenwald, MD, FACS, is a board-certified spine surgeon with extensive expertise performing microdiscectomy, a minimally invasive surgical procedure used to treat herniated discs that are pressing on spinal nerves. This precise technique involves removing only the small portion of the disc that is causing nerve compression, allowing patients to experience significant pain relief while preserving spinal stability. Dr. Greenwald uses state-of-the-art imaging and microsurgical tools to ensure minimal tissue disruption, reduced recovery time, and outstanding surgical outcomes. Patients throughout South Florida trust Dr. Greenwald for his skill, precision, and commitment to helping them regain mobility and live pain-free after debilitating disc-related conditions.
Book your Spine Care Consultation Today!


Desert Spine and Pain
Patient Centered & Partner Focused
Quick Links
Resources
Connect With Us
© Desert Spine and Pain. 2026. All Rights Reserved. Sitemap