Spine Surgery
Spinal Fusion Procedures
Stabilizing the Spine to Relieve Pain and Nerve Compression
When the spine becomes unstable due to degeneration, trauma, or deformity, a fusion procedure may be recommended. Fusion creates a permanent connection between two or more vertebrae, eliminating painful motion and supporting nerve decompression. At Desert Spine and Pain, neurosurgeon Dr. David L. Greenwald, M.D., FAANS, FACS offers a full range of fusion techniques—from traditional open approaches to advanced minimally invasive fusions. Each procedure is chosen based on the patient’s anatomy, condition, and goals.

Over 100 5-Star Reviews!

Fusion Procedures

Cervical Fusion
(Anterior or Posterior)

Lumbar Fusion
(Anterior, Posterior, PLIF, TLIF, LLIF)

Sacroiliac Joint Fusion
(MIS and Posterior/Lateral)
What Is Spinal Fusion?
In simple terms, spinal fusion surgery joins two or more bones in the spine together so they heal into a single, solid bone. From a more technical standpoint, spinal fusion involves disc space or posterolateral preparation, placement of bone graft or cage, and rigid fixation (screws/rods/plates) to promote arthrodesis through osteogenesis, osteoinduction, and osteoconduction.
Spine Fusion Surgeries
Cervical Fusion (Anterior or Posterior)
Cervical Fusion (Anterior or Posterior) is a surgical procedure that permanently joins two or more vertebrae in the neck to stabilize the spine and relieve nerve or spinal cord compression. It’s commonly used to treat conditions such as degenerative disc disease, spinal stenosis, spondylolisthesis, trauma, or instability after a herniated disc or prior surgery. The approach—anterior (front of the neck) or posterior (back of the neck)—depends on the location and cause of compression.
During an anterior cervical fusion, Dr. David Greenwald makes a small incision in the front of the neck to remove the damaged disc or bone spurs, then places a bone graft or interbody spacer between the vertebrae and secures it with a small plate and screws. In a posterior fusion, the incision is made along the back of the neck, and rods and screws are used to stabilize the spine after decompression. Both approaches allow the bone to fuse naturally over time, restoring alignment and preventing painful motion.
At Desert Spine and Pain, cervical fusion is performed using microsurgical, minimally invasive techniques that minimize tissue disruption and promote faster recovery. Patients typically experience immediate relief from arm pain and nerve symptoms, and over several months, the vertebrae fuse into a solid, stable structure that provides long-term strength and stability.
Lumbar Fusion (Anterior, Posterior, PLIF, TLIF, LLIF)
Lumbar Fusion—including Anterior (ALIF), Posterior (PLIF), Transforaminal (TLIF), and Lateral (LLIF) approaches—is a surgical procedure that permanently joins two or more vertebrae in the lower back to eliminate motion, restore spinal stability, and relieve nerve compression. It is commonly performed to treat degenerative disc disease, spondylolisthesis, spinal stenosis, fractures, or recurrent disc herniations. The difference between these techniques lies in how the surgeon accesses the spine.
At Desert Spine and Pain, Dr. David Greenwald tailors each fusion to the patient’s anatomy and condition:
ALIF (Anterior Lumbar Interbody Fusion): Access through the abdomen to remove the disc and insert an interbody cage with bone graft.
PLIF (Posterior Lumbar Interbody Fusion): Access through the back to remove the disc and insert cages on both sides of the spinal canal.
TLIF (Transforaminal Lumbar Interbody Fusion): Access through one side of the back, minimizing muscle disruption.
LLIF (Lateral Lumbar Interbody Fusion): Side approach through the flank, similar to the XLIF technique, avoiding major back muscles.
Each method uses bone grafts and titanium screws or rods to stabilize the spine while the vertebrae fuse naturally over time. These modern approaches—especially the minimally invasive techniques used at Desert Spine and Pain—allow for smaller incisions, reduced blood loss, less postoperative pain, and faster recovery. Most patients notice significant improvement in back and leg pain and can return to normal activities within a few weeks, with full fusion developing over several months for lasting spinal stability.
Sacroiliac Joint Fusion (MIS and Posterior/Lateral)
Sacroiliac Joint Fusion (MIS and Posterior/Lateral Approaches) is a specialized surgical procedure used to stabilize the sacroiliac (SI) joint, which connects the spine to the pelvis. When this joint becomes unstable or degenerates due to arthritis, trauma, or abnormal motion, it can cause chronic low back, hip, and buttock pain that often mimics sciatica. The goal of SI joint fusion is to eliminate painful movement by permanently joining the sacrum and ilium so they function as one solid unit.
At Desert Spine and Pain, Dr. David Greenwald performs both minimally invasive (MIS) and posterior/lateral fusion techniques. The MIS approach uses a small incision to insert specialized implants across the joint, promoting bone growth and long-term stability with minimal tissue disruption. The posterior or lateral approach allows targeted access to the joint for implant placement under fluoroscopic (X-ray) guidance, providing excellent accuracy while protecting surrounding nerves and muscles.
These modern techniques offer major advantages over traditional open surgery, including smaller incisions, less blood loss, reduced postoperative pain, and faster recovery. Most patients go home the same day or after an overnight stay and experience significant, lasting relief as the joint fuses naturally over time—restoring stability, alignment, and quality of life.
Speak to a Spine Specialist Today.
If you’ve been diagnosed with spinal instability or a degenerative condition, spinal fusion may be the key to lasting relief. Dr. Greenwald and his compassionate team will carefully evaluate your condition, discuss all available surgical options, and create a customized plan that best fits your needs. Every step you take toward advanced spine care brings you closer to stability, comfort, and restored function. Schedule your consultation today and discover how Dr. Greenwald’s expertise in spinal fusion can help you achieve long-term spinal health and relief.


Dr. David L. Greenwald, M.D., F.A.C.S.
Neurosurgeon | Spine Surgeon | Regenerative Medicine
Dr. David L. Greenwald, MD, FACS, is a board-certified spine surgeon with extensive experience performing spinal fusion procedures to stabilize the spine and relieve chronic pain caused by conditions such as degenerative disc disease, spondylolisthesis, scoliosis, and spinal fractures. By permanently joining two or more vertebrae, spinal fusion eliminates painful motion and restores stability to the affected area. Dr. Greenwald specializes in both traditional and minimally invasive fusion techniques—including TLIF, XLIF, PLIF, and ALIF—using advanced imaging and precision instrumentation to ensure optimal alignment and long-term success. His personalized approach helps patients throughout South Florida regain mobility, reduce pain, and return to active, pain-free living with confidence.
The Fusion Procedure: Step by Step

Anesthesia & positioning
You’re asleep under general anesthesia.

Access
Depending on the type (anterior, posterior, lateral), an incision is made in the neck, back, or side.

Disc removal
The damaged disc is removed, and bone surfaces are prepared.

Bone graft/cage placement
A bone graft or cage is placed to maintain space and allow bone to grow.

Stabilization
Screws, rods, or plates secure the area.

Closure
Incision is closed; patients walk within hours or days depending on the procedure.
Fusion Procedure Insights
Fusion Surgical Procedure Overview
Preparation: Endplate decortication and graft/cage sizing under fluoroscopic navigation.
Implant choice: Titanium, PEEK, or structural allograft cages; bone graft from iliac crest, allograft, or synthetic substitutes.
Fixation: Pedicle screws, rods, anterior plates, or lateral fixation systems.
Fusion biology: Use of autograft, allograft, BMP, or bone substitutes depending on patient profile.
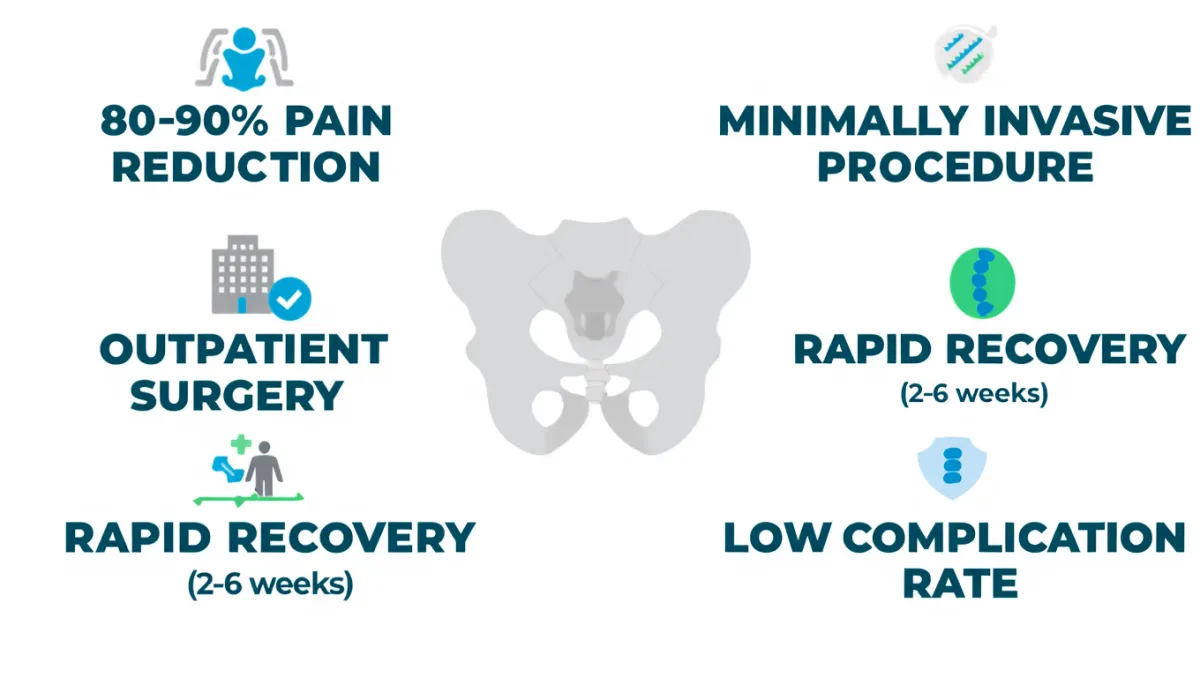
Benefits
Stabilizes painful, unstable motion segments
Relieves nerve compression when combined with decompression
Improves alignment and posture
Long-term success with high fusion rates
Minimally invasive options allow quicker recovery
Risks & Limitations
Infection, bleeding, anesthesia risks
Hardware complications or non-union (pseudoarthrosis)
Adjacent segment disease (wear above/below fused level)
Possible loss of motion at fused level(s)
Recovery varies depending on number of levels fused

Why Choose Desert Spine and Pain?
Comprehensive expertise: Dr. Greenwald performs the full range of fusion techniques, tailored to each patient
Minimally invasive focus: Smaller incisions, faster recovery, less pain
Conservative-first approach: Fusion is only recommended when other treatments fail
Trusted outcomes: High success rates and compassionate care in Phoenix
Contact Dr. Greenwald today for a Spine Consultation. Relief is a phone call away!
Recovery Timeline

Hospital stay
1–3 days for large fusions. Same day discharge on MIS

Weeks 1-2
Walking encouraged; incision healing

Weeks 2-6
Desk work possible, start gentle rehab

Weeks 6-12
Activity increases, PT focused on core and posture

Months 3-6
Most activities restored. Bone fusion consolidates

Months 6-12+
Fusion confirmed. Patients return to full life activity
Frequently Asked Questions
Will I lose mobility with a spinal fusion?
Yes, the fused segment no longer moves. But most patients notice little difference, especially when only 1–2 levels are fused.
How do I know if I need fusion?
Fusion is considered when instability, deformity, or recurrent disc problems cause persistent symptoms after conservative care.
What’s the difference between fusion and disc replacement?
Fusion eliminates motion at the treated level. Disc replacement preserves motion but isn’t suitable for everyone.
How long does it take for the bones to fuse?
Usually 6–12 months, depending on age, health, and whether you smoke (nicotine delays healing).
How does Desert Spine and Pain approach fusion differently?
We match the right fusion technique to your condition, using advanced MIS methods and neurosurgical precision for safer, faster recovery.
Book your Spine Care Consultation Today!


Desert Spine and Pain
Patient Centered & Partner Focused
Quick Links
Resources
Connect With Us
© Desert Spine and Pain. 2026. All Rights Reserved. Sitemap