Spine Surgery
Decompression Procedures
Opening up the Spine to Relieve Pressure on Nerves and the Spinal Cord
When nerves or the spinal cord are compressed by bone spurs, thickened ligaments, or herniated discs, patients may experience pain, numbness, tingling, weakness, or difficulty walking. Surgical decompression relieves this pressure by enlarging the spinal canal or nerve root exits. At Desert Spine and Pain, neurosurgeon Dr. David L. Greenwald, M.D., FAANS, FACS specializes in a variety of decompression procedures, performed with microsurgical and minimally invasive techniques whenever possible.

Over 100 5-Star Reviews!

Types of Spinal Decompression Surgery

Laminectomy

Foraminotomy

Corpectomy

Ulnar Nerve Decompression

Carpal Tunnel Release
What is a decompression surgery?
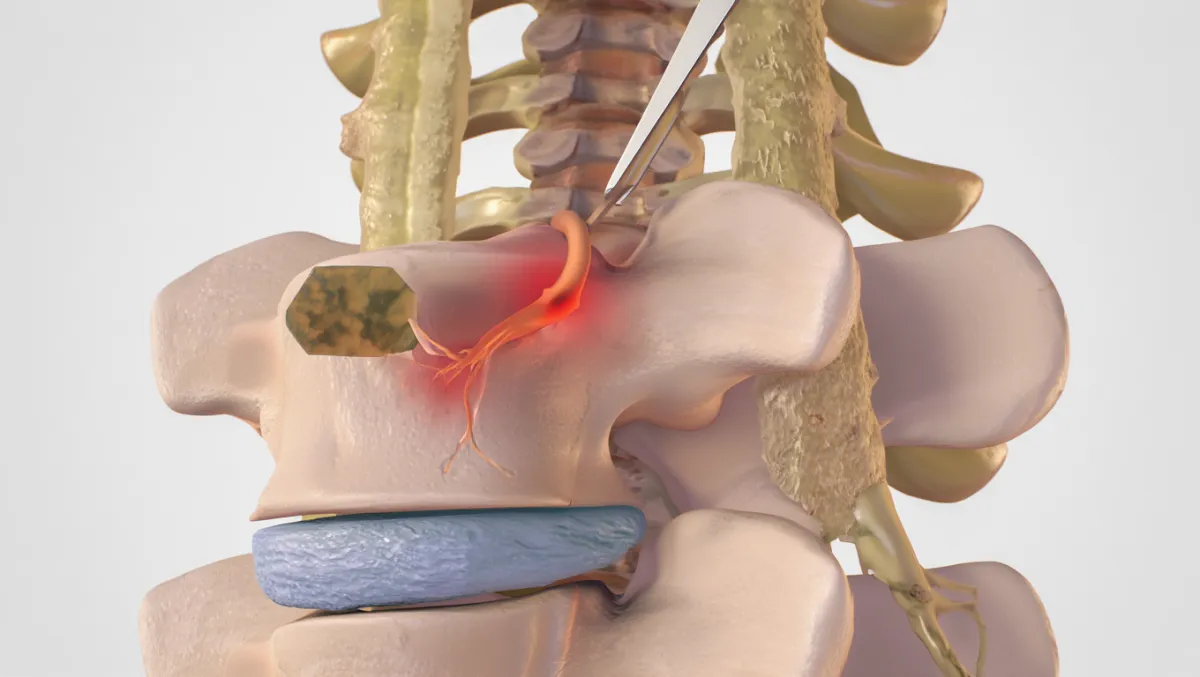
In a decompression surgery, we create more room for nerves in the spine by removing bone, ligaments, or disc material that’s pressing on them, thus decompressing the spine and providing relief. Decompression surgeries include laminectomy, laminotomy, foraminotomy, or discectomy, performed via open or MIS approaches, with or without stabilization, to relieve neural compression and restore canal and foraminal dimensions.
Spine Decompression Procedures
Laminectomy
Laminectomy is a surgical procedure that relieves pressure on the spinal cord and nerves by removing a small section of bone called the lamina—the back part of the vertebra that forms the spinal canal’s roof. This procedure is commonly performed to treat spinal stenosis, herniated discs, bone spurs, or degenerative arthritis that cause nerve compression and pain radiating into the arms or legs.
At Desert Spine and Pain, Dr. David Greenwald performs laminectomy using microsurgical and minimally invasive techniques to reduce muscle disruption and speed recovery. Through a small incision, the affected lamina and any thickened ligaments or bone overgrowths are carefully removed to decompress the spinal canal and free the nerves. This often results in immediate relief from nerve pain, leg weakness, and numbness.
Depending on the patient’s needs, a laminectomy may be combined with spinal fusion or stabilization if there is significant instability or deformity. Most patients are able to walk within hours after surgery, return home the same or next day, and resume normal activities within a few weeks—experiencing lasting improvement in pain and mobility with less downtime and scarring than traditional open surgery.
Foraminotomy
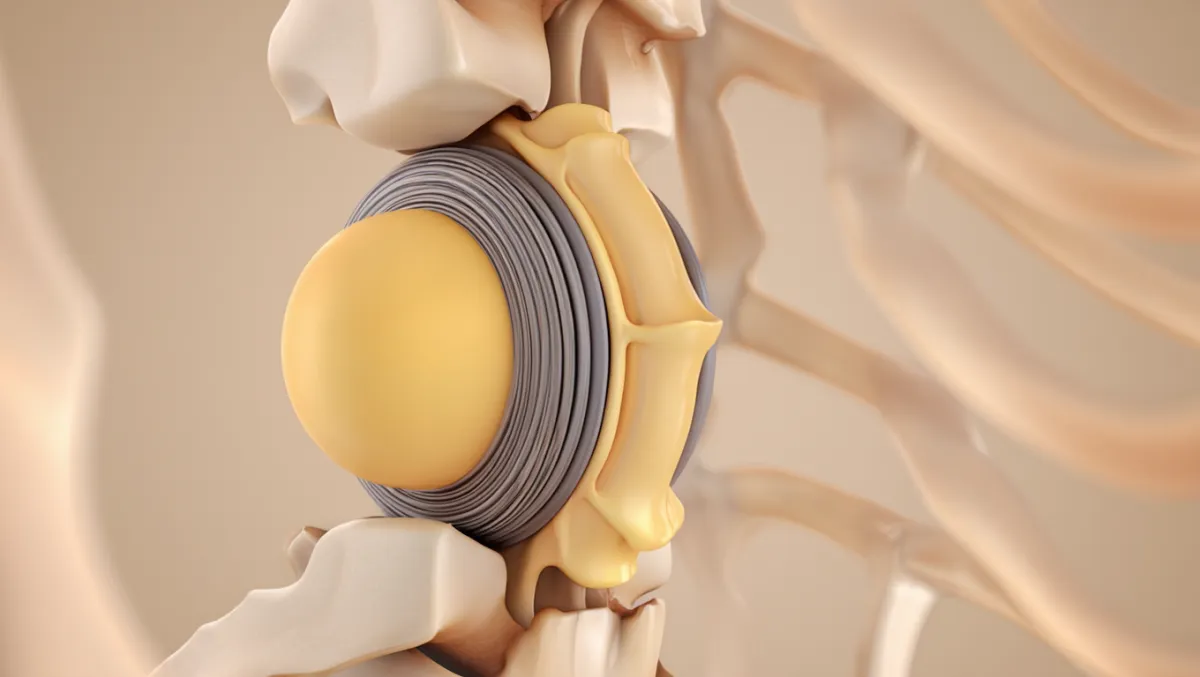
Foraminotomy is a surgical procedure that relieves pressure on spinal nerves by enlarging the foramen—the small openings between vertebrae where nerves exit the spinal canal. When these openings become narrowed due to arthritis, bone spurs, herniated discs, or degenerative changes, nerves can become compressed, leading to pain, numbness, tingling, or weakness that radiates into the arms or legs.
At Desert Spine and Pain, Dr. David Greenwald performs foraminotomy using microsurgical and minimally invasive techniques to achieve precise decompression with minimal tissue disruption. Through a small incision, specialized instruments are used to remove small portions of bone, thickened ligaments, or disc material that are compressing the nerve. This creates more space for the nerve to move freely and function normally.
Most patients experience immediate relief of nerve-related pain and a faster recovery compared to traditional open surgery. Foraminotomy can be performed alone or combined with other decompression procedures such as laminectomy or discectomy, depending on the cause of compression. Patients treated at Desert Spine and Pain benefit from smaller incisions, less postoperative pain, and shorter recovery times, allowing them to return to normal activity with restored comfort and mobility.
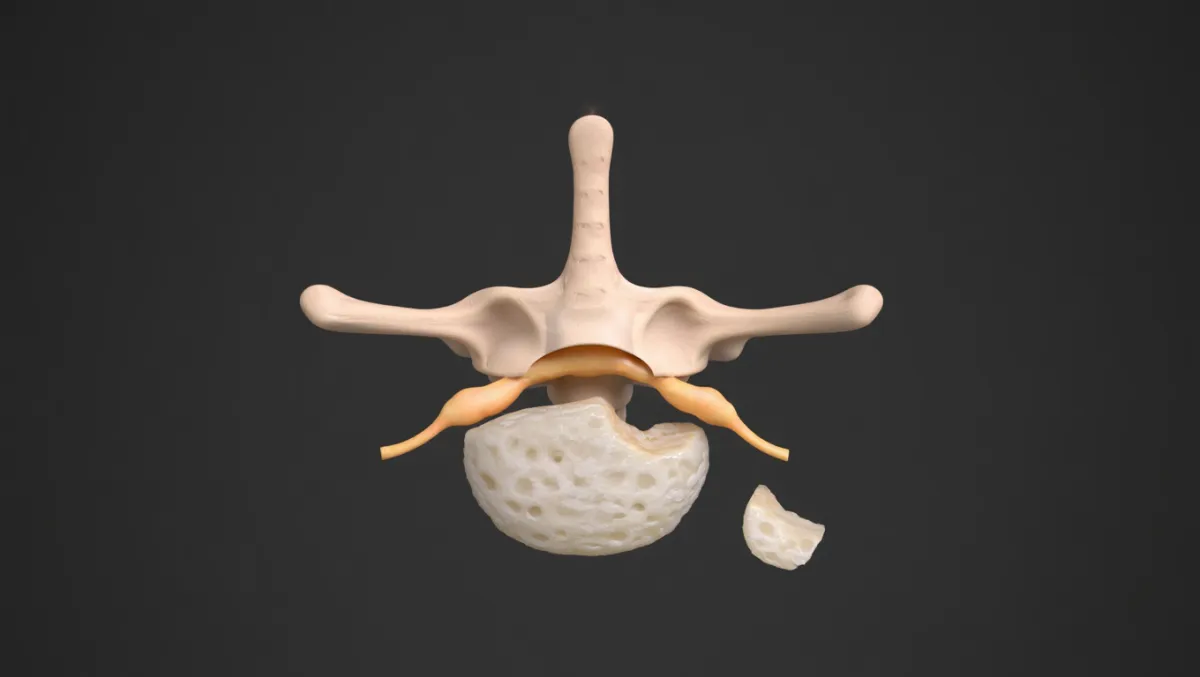
Corpectomy
Corpectomy is an advanced spinal surgery performed to relieve pressure on the spinal cord and nerves by removing part or all of a vertebral body (corpus) and the discs above and below it. This procedure is typically used to treat severe spinal stenosis, spinal cord compression, fractures, tumors, infections, or deformities that cannot be adequately addressed with smaller decompression surgeries. By removing the diseased bone and disc material, the spinal canal is widened, and nerve function can be restored.
At Desert Spine and Pain, Dr. David Greenwald performs corpectomy with microsurgical precision and advanced stabilization techniques. After removing the affected vertebral body, the space is reconstructed with a titanium cage or bone graft and stabilized using plates, screws, or rods to maintain alignment and allow the bones to fuse. This restores both height and stability to the spine.
Although corpectomy is a more complex procedure, it provides direct decompression of the spinal cord, offering significant relief for patients with severe compression or instability. Using modern imaging and minimally invasive principles whenever possible, Dr. Greenwald ensures safe, effective decompression with optimal outcomes. Patients typically notice improvement in pain, strength, and mobility, followed by gradual fusion and long-term spinal stability.
Ulnar Nerve Decompression
Ulnar Nerve Decompression is a surgical procedure used to relieve pressure on the ulnar nerve, which runs from the neck through the elbow (commonly known as the “funny bone”) and into the hand. Compression of this nerve—often at the elbow in a condition called cubital tunnel syndrome—can cause numbness, tingling, and weakness in the ring and little fingers, hand, and forearm. The goal of surgery is to restore normal nerve function and prevent permanent damage.
At Desert Spine and Pain, Dr. David Greenwald performs ulnar nerve decompression using microsurgical and minimally invasive techniques. Through a small incision along the inner elbow, the tight tissues compressing the nerve (such as fascia or ligaments) are carefully released, allowing the nerve to glide freely. In some cases, the nerve may be transposed (moved) to a more protected position in front of the elbow to prevent future irritation.
This outpatient procedure typically results in immediate improvement of tingling and pain, with hand strength returning gradually as the nerve heals. Most patients return to light activities within a few days and experience long-lasting relief. The minimally invasive approach used at Desert Spine and Pain ensures smaller incisions, faster recovery, and excellent functional outcomes.
Carpal Tunnel Release
Carpal Tunnel Release is a surgical procedure that relieves pressure on the median nerve as it passes through the carpal tunnel in the wrist. When this tunnel becomes too tight—often due to repetitive motion, inflammation, or swelling of surrounding tissues—it can cause numbness, tingling, pain, or weakness in the hand and fingers, a condition known as carpal tunnel syndrome. The goal of surgery is to restore normal nerve function and hand strength by freeing the compressed nerve.
At Desert Spine and Pain, Dr. David Greenwald performs both open and endoscopic carpal tunnel release techniques, depending on each patient’s needs. During the procedure, a small incision is made in the wrist or palm to cut the transverse carpal ligament, which forms the “roof” of the tunnel. This immediately reduces pressure on the median nerve, allowing it to heal.
Most patients experience rapid improvement in numbness, tingling, and grip strength following surgery. Because minimally invasive and endoscopic techniques are used whenever possible, recovery is typically quick—many patients return to light activities within days and full use of the hand within a few weeks. This safe, highly effective procedure helps restore comfort, coordination, and quality of life for patients suffering from carpal tunnel syndrome.
The Decompression Surgery: Step by Step

Anesthesia
You’re asleep under general anesthesia.

Incision
Small incision in the neck, mid-back, or lower back depending on site.

Bone/ligament removal
Lamina, ligamentum flavum, or bone spurs are trimmed away.

Disc fragment removal (if needed)
Herniated disc material is taken out.

Nerve decompression
The spinal cord and/or nerve roots are freed.

Stabilization (if required)
Screws/rods/cages may be added if fusion is needed.

Closure
Incision closed; many patients walk the same day or next.
Decompression Surgery Insights
Decompression Procedure Surgical Steps
Docking: MIS tubular retractor or open exposure depending on pathology.
Bone removal: Drill/Kerrisons for laminectomy or laminotomy; medial facetectomy for foraminotomy.
Disc removal: Pituitary rongeurs remove herniated nucleus fragments.
Laminoplasty (when used): Hinge drilled on one side of lamina; lamina opened and secured with plates.
Fusion decision: Based on instability, slip, or deformity.
Benefits
Relieves pain, numbness, weakness, and walking limitations
Improves function and quality of life
Can be performed with small incisions using MIS
Options for motion preservation (laminoplasty, Coflex) when fusion not required
High success rates in properly selected patients
Risks & Limitations
Infection, bleeding, CSF leak
Nerve or spinal cord injury (rare with neurosurgical precision)
Scar tissue formation, recurrent stenosis
Instability if too much bone removed (fusion may be needed)
Not a cure for all back pain (best for nerve-related symptoms)
Why Choose Desert Spine and Pain?
Expert neurosurgeon: Dr. Greenwald brings precision and safety to every decompression procedure
MIS focus: Small incisions, less pain, faster recovery whenever possible
Personalized plans: Conservative-first philosophy; surgery tailored to condition and goals
Comprehensive care: Rehab and follow-up integrated into your treatment plan
Contact Dr. Greenwald today to schedule your Spine Pain Consultation. Pain relief is just a phone call away! Call now!
Recovery Timeline

0-2 Days
Walking within hours; hospital stay 0–2 nights

Weeks 1-2
Wound care, light walking encouraged

Weeks 2-6
Desk work resumed; PT often starts

Weeks 6-12
Activity gradually increased

Months 3-6
Strong functional recovery; improved walking tolerance

Months 6-12+
Fusion consolidation if performed; long-term results achieved
Book a Spine Consultation Today.
If you’re struggling with persistent back or leg pain, tingling, or weakness, a spinal decompression procedure may be the key to relief. Dr. Greenwald and his caring team will carefully assess your condition, review imaging, and determine the most effective treatment for your needs. Every step you take toward decompressing and healing your spine brings you closer to renewed comfort and freedom of movement. Schedule your consultation today and take the first step toward lasting relief and restored spinal health.


Dr. David L. Greenwald, M.D., F.A.C.S.
Neurosurgeon | Spine Surgeon | Regenerative Medicine
Dr. David L. Greenwald, MD, FACS, is a board-certified spine surgeon specializing in decompression procedures, which are designed to relieve pressure on the spinal nerves caused by conditions such as spinal stenosis, herniated discs, or bone spurs. These procedures—performed using advanced, minimally invasive techniques—remove small portions of bone or disc material to restore space within the spinal canal, easing nerve compression and reducing pain, numbness, and weakness. Dr. Greenwald’s precise and patient-focused approach minimizes tissue disruption, shortens recovery time, and delivers long-lasting relief. Patients throughout South Florida trust his expertise to restore comfort, mobility, and quality of life through safe and effective spinal decompression surgery.
Frequently Asked Questions
What’s the difference between a laminectomy and a laminotomy?
Laminectomy removes the entire lamina; laminotomy removes part of it. Both decompress nerves but differ in how much bone is removed.
Will decompression cure my back pain?
It’s most effective for nerve-related symptoms (leg/arm pain, numbness, weakness). Back pain alone may not always improve.
Do all decompressions require fusion?
No. Fusion is only added if instability exists or if too much bone must be removed.
How soon can I walk after decompression surgery?
Most patients walk the same day or next, with gradual increase in distance.
How does Desert Spine and Pain perform decompression differently?
We emphasize neurosurgical precision, minimally invasive tools, and motion-preserving techniques whenever appropriate.
Book your Spine Care Consultation Today!


Desert Spine and Pain
Patient Centered & Partner Focused
Quick Links
Resources
Connect With Us
© Desert Spine and Pain. 2026. All Rights Reserved. Sitemap