Stenosis Surgery
Cervical Stenosis Surgery
Relieving Spinal Cord and Nerve Pressure in the Neck
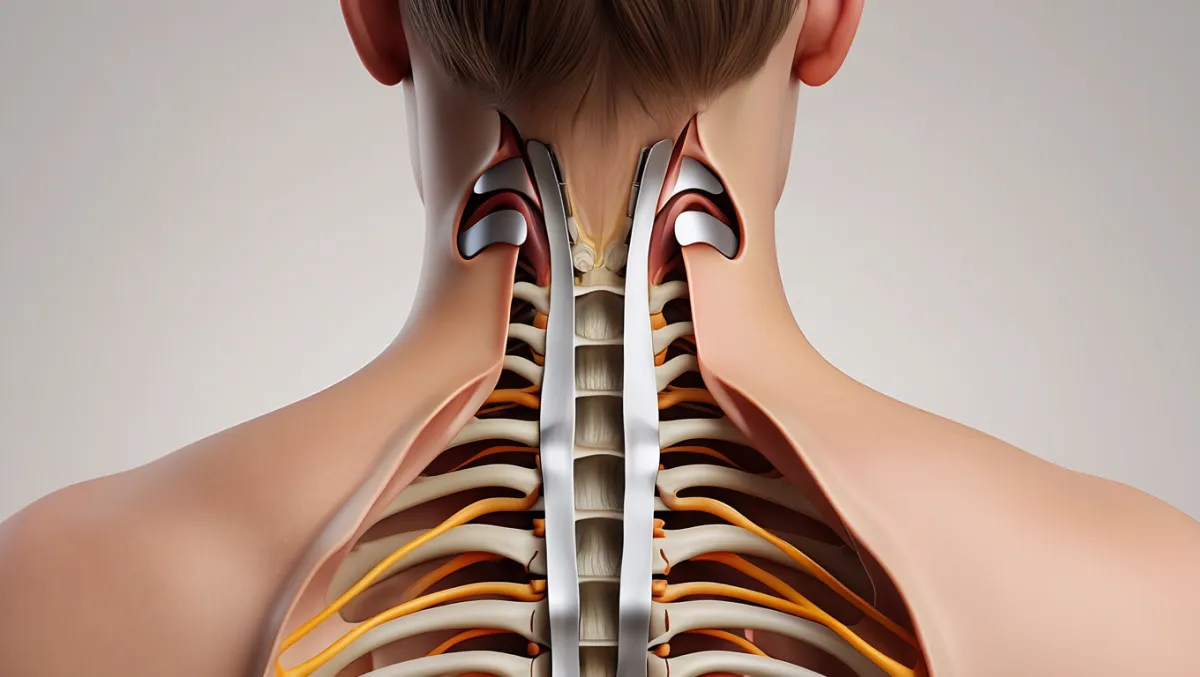
Cervical stenosis occurs when the spinal canal in the neck narrows, compressing the spinal cord or nerves. This can cause neck pain, arm pain, numbness, weakness, balance problems, and in severe cases, myelopathy (spinal cord dysfunction). When conservative care isn’t enough, cervical stenosis surgery may be necessary to decompress the spinal cord and stabilize the spine. At Desert Spine and Pain, neurosurgeon Dr. David L. Greenwald, M.D., FAANS, FACS specializes in both anterior and posterior surgical approaches, choosing the safest and most effective technique based on your condition.

Over 100 5-Star Reviews!

What Is Cervical Stenosis Surgery?
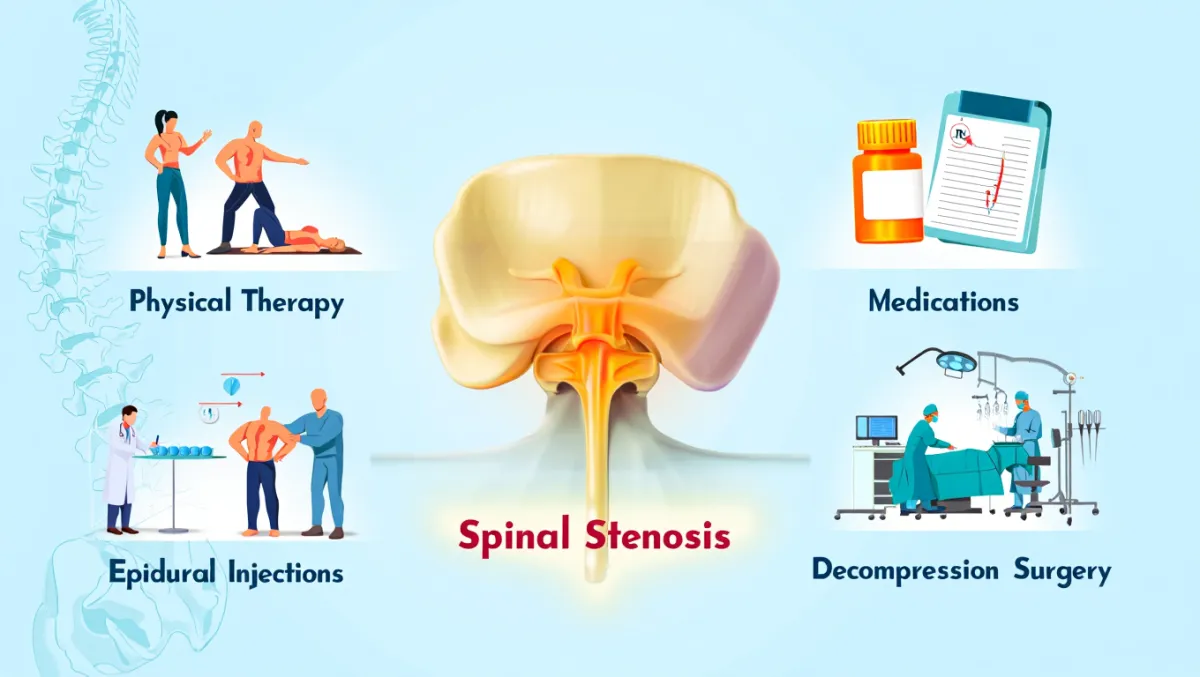
In simple terms: We make space for the spinal cord and nerves by removing bone, ligaments, or disc material that is narrowing the canal. Sometimes we also stabilize the spine with fusion or disc replacement.
Scientifically: Surgical decompression of cervical stenosis may involve anterior cervical discectomy and fusion (ACDF), anterior cervical disc replacement, laminoplasty, or posterior laminectomy/laminotomy with or without fusion. The goal is to restore canal diameter, relieve cord/nerve compression, and preserve or restore spinal alignment.
Conditions Treated
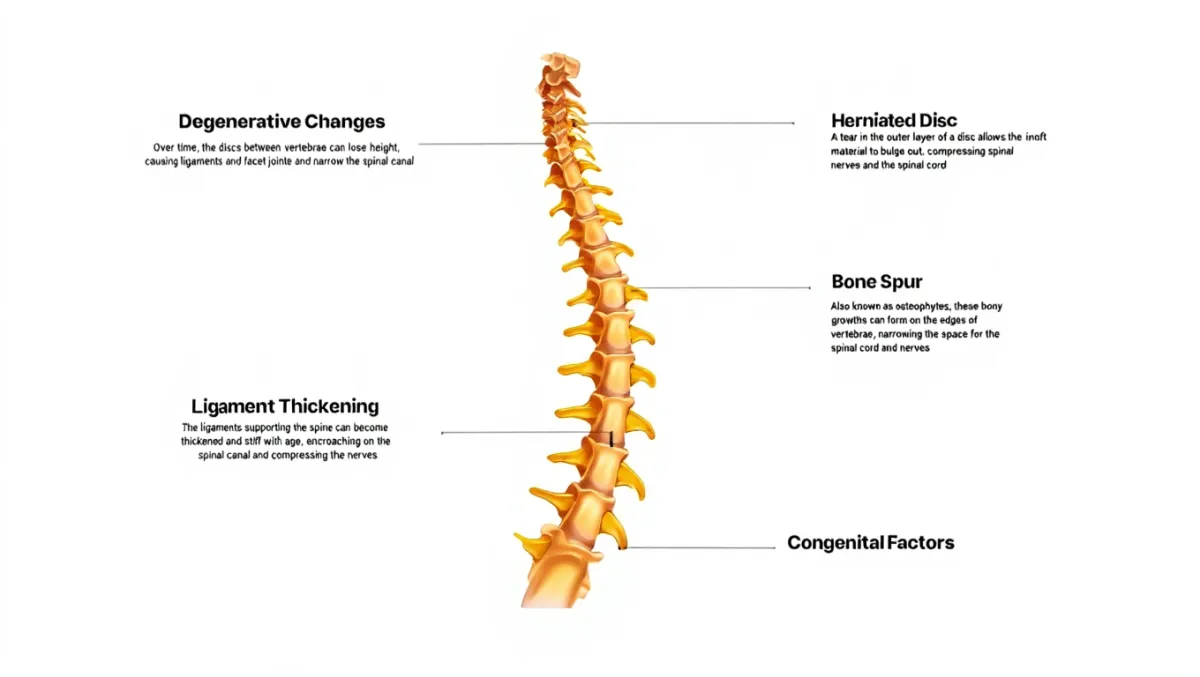
Cervical spinal stenosis
Cervical myelopathy (cord compression with weakness, clumsiness, or balance problems)
Cervical radiculopathy (arm pain, numbness, tingling)
Disc herniations or bone spurs narrowing the cervical canal
Multi-level degenerative changes causing both cord and nerve compression
Types of Cervical Stenosis Surgery
1. Anterior Cervical Discectomy and Fusion (ACDF)
Removes disc and bone spurs through a small incision in the front of the neck
Fusion stabilizes the spine with bone graft and plate
2. Anterior Cervical Disc Replacement
Removes diseased disc and replaces it with an artificial disc
Preserves motion instead of fusing
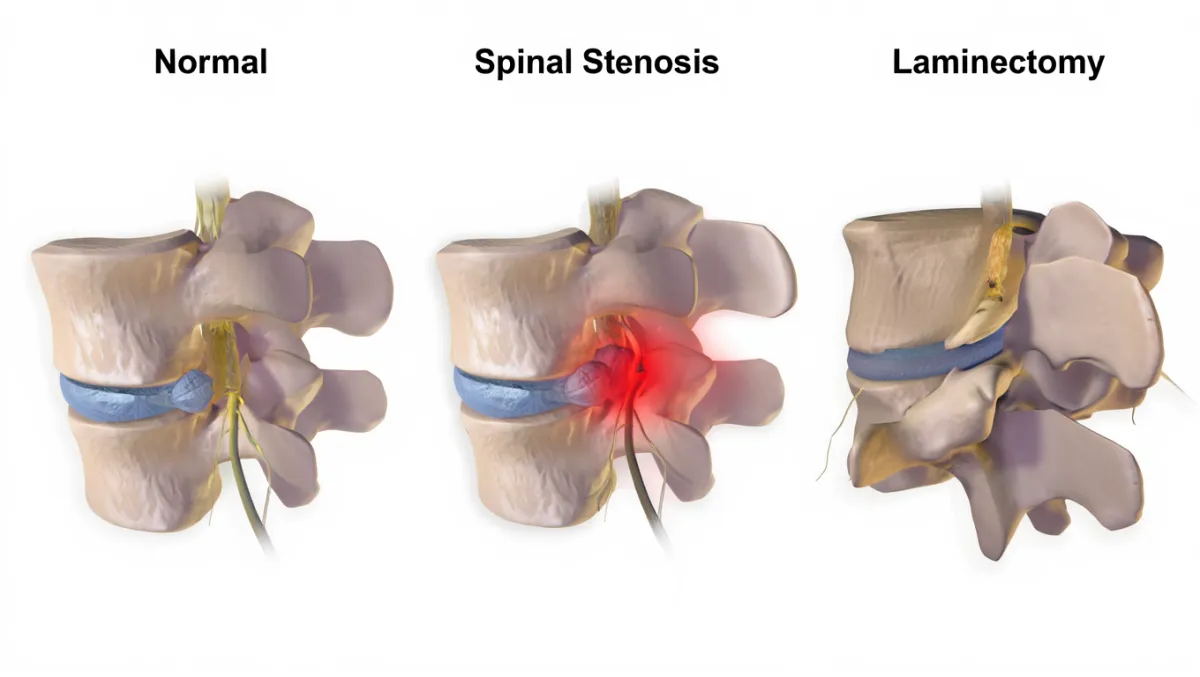
3. Posterior Laminectomy / Laminotomy
Removes part or all of the lamina (back of the vertebra) to decompress the cord and nerves
May be combined with fusion for stability in certain cases
4. Cervical Laminoplasty
Expands the spinal canal by hinging open the lamina and securing it with plates
Preserves motion while relieving compression (used mainly for multi-level stenosis)
The Procedure: Step by Step
Plain-English Overview
Anesthesia & positioning: You’re asleep under general anesthesia.
Incision: Small incision in the front or back of the neck, depending on approach.
Decompression: Disc material, bone spurs, or lamina are removed to relieve pressure.
Stabilization (if needed): Fusion or disc replacement is performed to maintain alignment and stability.
Closure: Incision closed; most patients walk the same or next day.
Surgeon-Level Detail
Anterior approach: Smith-Robinson exposure; microsurgical discectomy; PLL resection; cage with graft and anterior plate, or artificial disc placement.
Posterior approach: Midline incision; laminotomy or laminectomy with drill/Kerrisons; foraminotomies if needed; fusion with lateral mass/pedicle screws in cases of instability or kyphosis.
Laminoplasty option: Hinge side created with drill; lamina lifted open and secured with mini-plates.
Benefits of Cervical Stenosis Surgery
Relieves cord and nerve compression
Prevents progression of myelopathy (weakness, clumsiness, balance issues)
Restores walking ability and arm strength in many patients
Small incisions with MIS and motion-preserving options available
Can be tailored for single- or multi-level disease
Risks & Limitations
Difficulty swallowing (temporary dysphagia) with anterior surgery
Hoarseness (recurrent laryngeal nerve irritation, often temporary)
Infection, bleeding, nerve injury, CSF leak (rare with microsurgical precision)
Non-union (in fusion cases)
Reduced neck mobility if multiple levels fused
Recovery Timeline
Day 0–1: Walking same day or next; many go home in 24–48 hours
Weeks 1–2: Mild soreness; swallowing difficulty possible with anterior approach
Weeks 2–6: Desk work and light activity resumed
6–12 weeks: Begin or continue physical therapy; fusion or implant stabilizing
3–6 months: Improved balance, strength, and function
6–12 months: Fusion or long-term stability confirmed with imaging
Why Choose Desert Spine and Pain?
Expert neurosurgeon: Dr. Greenwald is highly skilled in both anterior and posterior cervical stenosis surgery
Advanced techniques: MIS and motion-preserving procedures available
Comprehensive care: Conservative treatments always considered first
Compassionate approach: We take time to explain the process and ease fears about surgery
Frequently Asked Questions
How do I know if I need cervical stenosis surgery?
If you have progressive weakness, clumsiness, or balance issues—or severe arm/neck pain not relieved by conservative care—you may need surgery.
What’s the difference between anterior and posterior surgery?
Anterior is best for 1–2 level disease in the front of the spine. Posterior is often chosen for multi-level stenosis or when cord compression extends across several levels.
Will I lose neck motion?
Fusion reduces motion at the treated levels, but disc replacement or laminoplasty may preserve movement.
How soon will I feel better?
Arm pain and numbness often improve quickly. Balance, coordination, and hand function improve gradually over months.
How does Desert Spine and Pain perform cervical stenosis surgery differently?
We use neurosurgical precision, minimally invasive approaches, and a patient-first philosophy to maximize safety, preserve motion when possible, and ensure lasting results.




Dr. David L. Greenwald, MD
Neuro-Spine Surgeon

Call Now!
Desert Spine and Pain
A Spine Specialist is standing by.
Relief is just a phone call away!
Available Around the Clock.
Phone: (602) 566-9500
Email: [email protected]
Contact Us

Your Journey Begins with us.
If you’re suffering from neck pain, weakness, or loss of coordination caused by cervical spinal stenosis, expert evaluation and treatment can prevent progression and restore comfort. Dr. Greenwald and his caring team will perform a detailed assessment, explain your options, and determine whether Cervical Stenosis Surgery is right for you. Every step you take toward proper spine care brings you closer to strength, mobility, and relief. Schedule your consultation today and discover how Dr. Greenwald’s advanced surgical expertise can help you regain control of your spine health and quality of life.

Voted Best Spine Doctor
Over 30 Years Experience in Orthopedic & Neuro Spine Surgeries.

Dr. David L. Greenwald, M.D., F.A.C.S.
Neurosurgeon | Spine Surgeon | Regenerative Medicine
Dr. David L. Greenwald, MD, FACS, is a board-certified spine surgeon specializing in Cervical Stenosis Surgery, a procedure designed to relieve spinal cord or nerve compression in the neck caused by narrowing of the cervical spinal canal. Cervical spinal stenosis can lead to neck pain, arm weakness, numbness, balance problems, or even difficulty with coordination if left untreated. Dr. Greenwald performs both traditional and minimally invasive decompression surgeries, including laminectomy, laminoplasty, or foraminotomy, depending on each patient’s needs. With precision-guided imaging and a patient-centered approach, he ensures safe, effective decompression to preserve spinal stability and restore neurological function. Patients throughout South Florida trust Dr. Greenwald for his expertise, compassionate care, and dedication to helping them return to a pain-free, active lifestyle.
Book your Spine Care Consultation Today!


Desert Spine and Pain
Patient Centered & Partner Focused
Quick Links
Resources
Connect With Us
© Desert Spine and Pain. 2026. All Rights Reserved. Sitemap