Stenosis
Lumbar Stenosis Surgery
Restoring Space for Pinched Nerves in the Lower Back
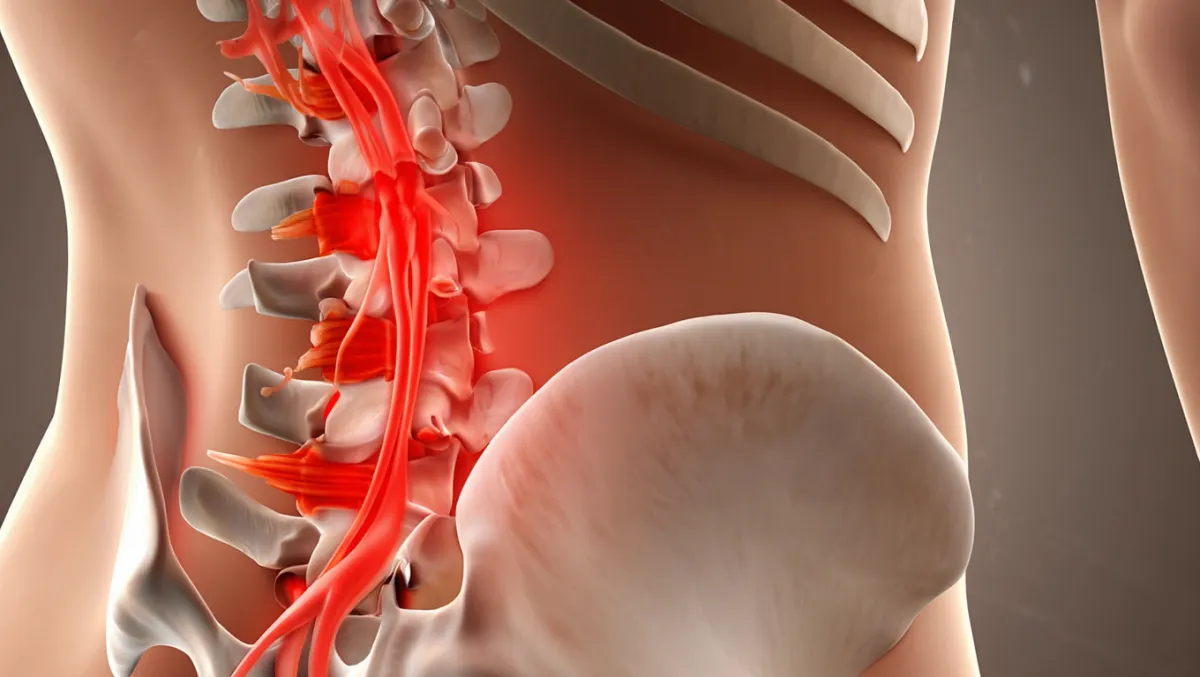
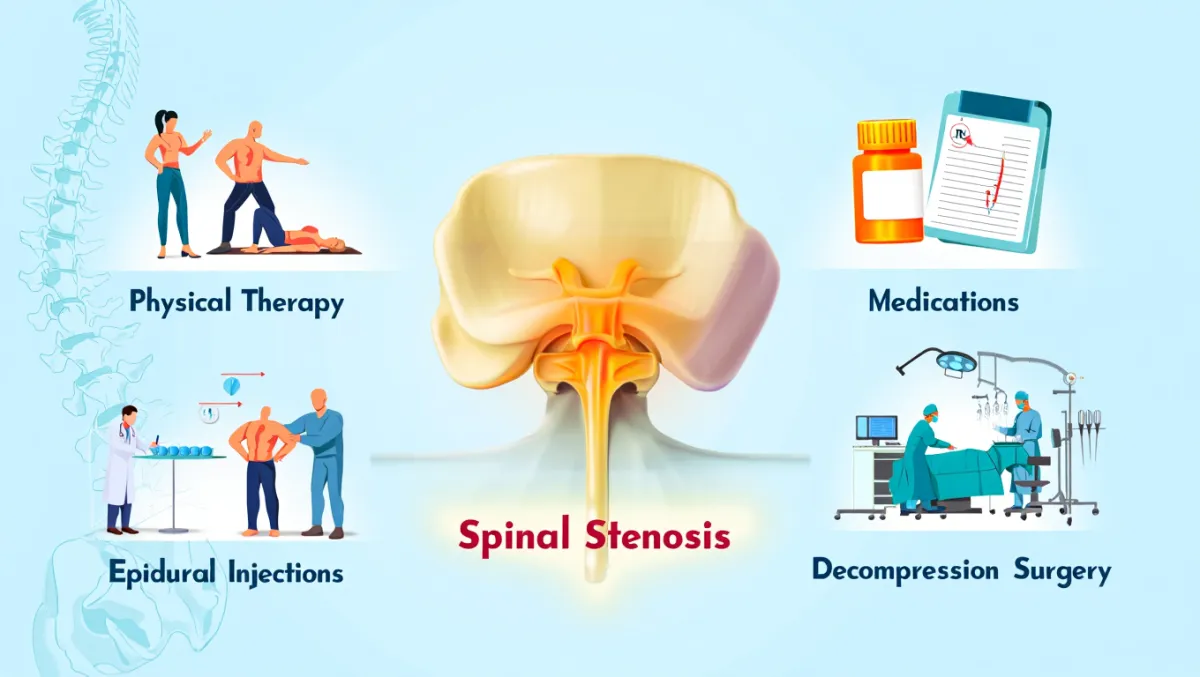
Lumbar spinal stenosis occurs when the spinal canal or foramina in the lower back narrow, squeezing the spinal nerves. This often causes leg pain, numbness, tingling, weakness, or cramping when standing or walking—a condition called neurogenic claudication. When conservative care (PT, medications, injections) no longer provides relief, lumbar stenosis surgery is recommended to decompress the nerves and restore mobility. At Desert Spine and Pain, neurosurgeon Dr. David L. Greenwald, M.D., FAANS, FACS uses advanced minimally invasive decompression techniques, and when necessary, fusion procedures to stabilize the spine.

Over 100 5-Star Reviews!

What Is Lumbar Stenosis Surgery?
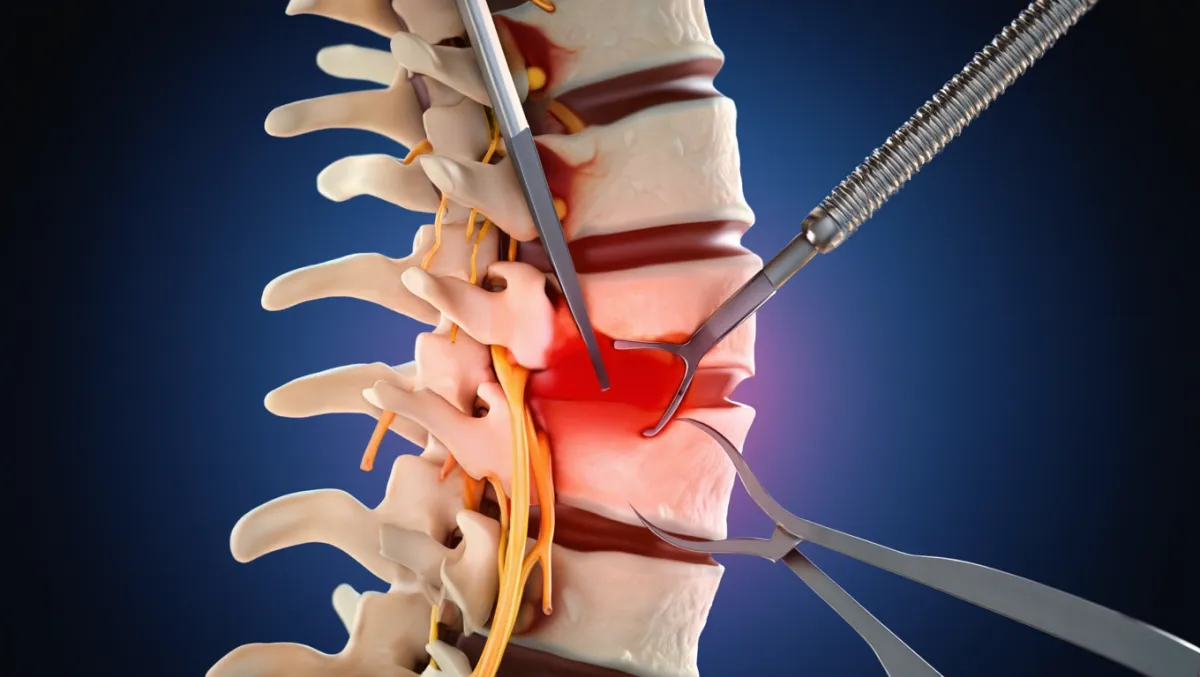
In simple terms: We create more space in the lower back by removing bone, ligaments, or disc material that are compressing nerves.
Scientifically: Lumbar decompression may include laminectomy, laminotomy, foraminotomy, or discectomy to enlarge the spinal canal and foramina. When instability exists, procedures like TLIF or XLIF combine decompression with stabilization.

Conditions Treated
Lumbar spinal stenosis
Neurogenic claudication (pain with walking, relieved by sitting/flexion)
Radiculopathy (leg pain, numbness, tingling)
Spondylolisthesis with instability
Recurrent disc herniations with stenosis
Combined stenosis and degenerative deformity

Types of Lumbar Stenosis Surgery
1. Laminectomy
Removal of lamina and ligamentum flavum to enlarge spinal canal.
Classic treatment for lumbar stenosis.
Learn more → Laminectomy / Foraminotomy
2. Laminotomy / Foraminotomy
Removes part of lamina or enlarges foraminal exit for nerves.
Minimally invasive with smaller incision.
3. Decompression with Fusion
Used when instability is present or created by decompression.
Options: TLIF, PLIF, XLIF.
4. Coflex Interlaminar Stabilization
Motion-preserving alternative after decompression in select patients.
Learn more → Coflex Placement
The Lumbar Stenosis Procedure: Step by Step
Plain-English Overview
Anesthesia & positioning: You’re asleep under general anesthesia, lying face down.
Small incision(s): Made in the lower back at affected level(s).
Decompression: Lamina, ligamentum flavum, and bone spurs removed to open canal.
Nerve release: Nerve roots and dura freed from compression.
Stabilization (if needed): Screws, rods, or cages added to prevent instability.
Closure: Small sutures or glue used; many walk the same day.
Surgeon-Level Detail
Docking: MIS tubular retractor positioned over lamina; microscope provides magnification.
Bone removal: High-speed drill and Kerrisons thin lamina; ligamentum flavum resected.
Foraminotomy: Medial facetectomy widens nerve root exit.
Fusion decision: Based on slip, motion, or facet removal; interbody cage + pedicle screws if instability present.
Closure: Meticulous hemostasis; layered closure.

Benefits of Lumbar Stenosis Surgery
Reliable relief of leg pain, numbness, and cramping
Improved walking and standing tolerance
Minimally invasive options mean smaller scars and faster recovery
Motion-preserving options available in select cases
High long-term success when diagnosis is correct
Risks & Limitations
Infection, bleeding, CSF leak
Nerve injury (rare with neurosurgical precision)
Scar tissue or recurrent stenosis
Possible spinal instability requiring fusion
Longer recovery if multi-level decompression/fusion performed
Recovery Timeline
Day 0–1: Walking same or next day; most stay 0–2 nights
Weeks 1–2: Light activity, daily walking encouraged
Weeks 2–6: Desk work possible; PT often begins
6–12 weeks: Progressive activity; restrictions lifted gradually
3–6 months: Improved mobility, leg strength, and function
6–12 months: Fusion (if performed) confirmed on X-rays; long-term recovery achieved
Why Choose Desert Spine and Pain?
Neurosurgeon-led expertise: Dr. Greenwald has decades of experience in lumbar decompression and fusion
Advanced MIS techniques: Smaller incisions, less muscle damage, quicker recovery
Full spectrum of options: From decompression alone to fusion or Coflex, all tailored to the patient
Compassionate care: We guide patients through diagnosis, surgery, and rehab with clarity and support
Frequently Asked Questions
How do I know if I need lumbar stenosis surgery?
If walking or standing causes leg pain/numbness that improves with sitting/flexing, and conservative care has failed, surgery may help.
What’s the difference between laminectomy and laminotomy?
Laminectomy removes the whole lamina; laminotomy removes part. Both create more space for nerves.
Will I need a fusion with decompression?
Not always. Fusion is added only when instability exists or is created during surgery.
How soon can I walk after surgery?
Most patients walk the same day, with steady improvement in leg symptoms.
How does Desert Spine and Pain perform lumbar stenosis surgery differently?
We use microsurgical and minimally invasive decompression, reserving fusion for when it’s truly necessary, always with neurosurgical precision.




Dr. David L. Greenwald, MD
Neuro-Spine Surgeon

Call Now!
Desert Spine and Pain
A Spine Specialist is standing by.
Relief is just a phone call away!
Available Around the Clock.
Phone: (602) 566-9500
Email: [email protected]
Contact Us

Book a Consultation.
If you’re experiencing pain, numbness, or weakness in your legs due to lumbar spinal stenosis, expert surgical care can make all the difference. Dr. Greenwald and his compassionate team will evaluate your condition, review imaging, and determine whether Lumbar Stenosis Surgery is the best solution for your needs. Every step you take toward advanced spine care brings you closer to comfort, strength, and renewed independence. Schedule your consultation today and let Dr. Greenwald help you walk, move, and live without pain.

Voted Best Spine Doctor
Over 30 Years Experience in Orthopedic & Neuro Spine Surgeries.

Dr. David L. Greenwald, M.D., F.A.C.S.
Neurosurgeon | Spine Surgeon | Regenerative Medicine
Dr. David L. Greenwald, MD, FACS, is a board-certified spine surgeon specializing in Lumbar Stenosis Surgery, a procedure designed to relieve pressure on spinal nerves in the lower back caused by narrowing of the spinal canal. This condition, known as lumbar spinal stenosis, can lead to leg pain, numbness, weakness, and difficulty walking. Dr. Greenwald performs both traditional and minimally invasive decompression surgeries—such as laminectomy or laminotomy—to remove bone spurs or thickened ligaments that compress the nerves. His precision-guided techniques minimize tissue disruption, reduce recovery time, and help patients throughout South Florida achieve lasting relief, improved mobility, and restored quality of life.
Book your Spine Care Consultation Today!


Desert Spine and Pain
Patient Centered & Partner Focused
Quick Links
Resources
Connect With Us
© Desert Spine and Pain. 2026. All Rights Reserved. Sitemap