Spine Surgery
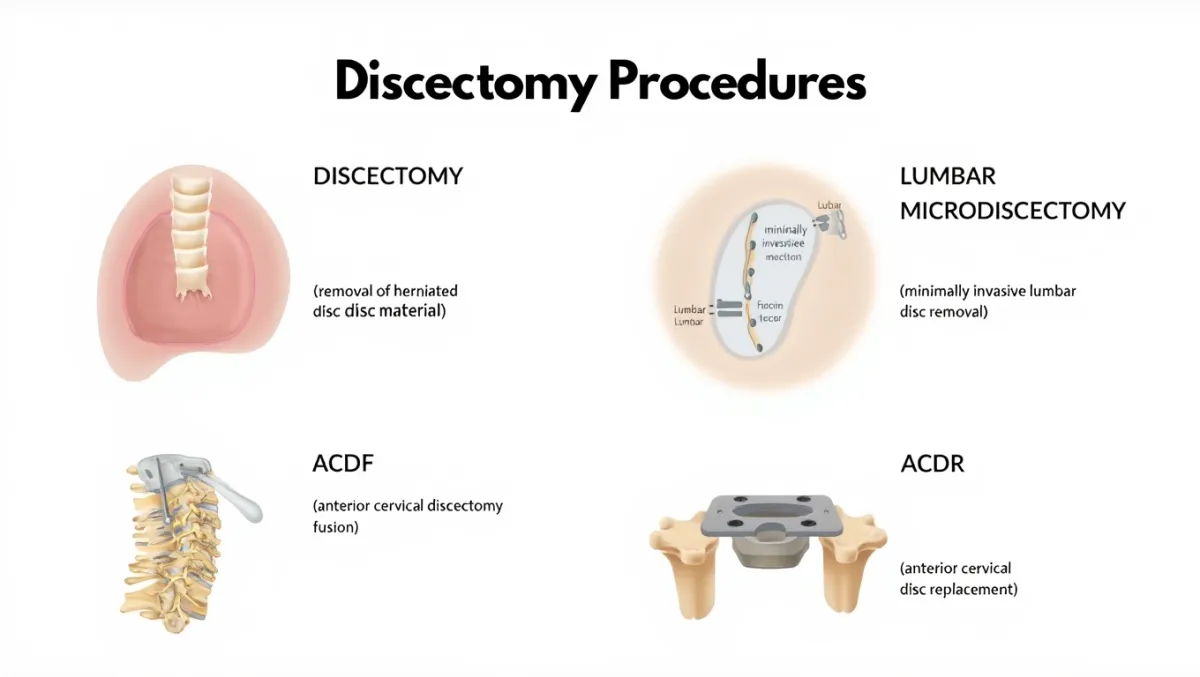
Discectomy Procedures
Surgically Removing Damaged Disc Material to Relieve Nerve Compression
A discectomy is a surgical procedure to remove part of a spinal disc that is pressing on a nerve or the spinal cord. At Desert Spine and Pain, discectomies are performed using minimally invasive microsurgical techniques, which means smaller incisions, less muscle disruption, and faster recovery. Led by Dr. David L. Greenwald, M.D., FAANS, FACS, one of the country’s top neurosurgeons, we specialize in multiple types of discectomy procedures tailored to each patient’s needs.

Over 100 5-Star Reviews!

Types of Discectomy Procedures

Discectomy

Lumbar Microdiscectomy

Anterior Cervical Discectomy Fusion (ACDF)

Anterior Cervical Discectomy with Disc Replacement
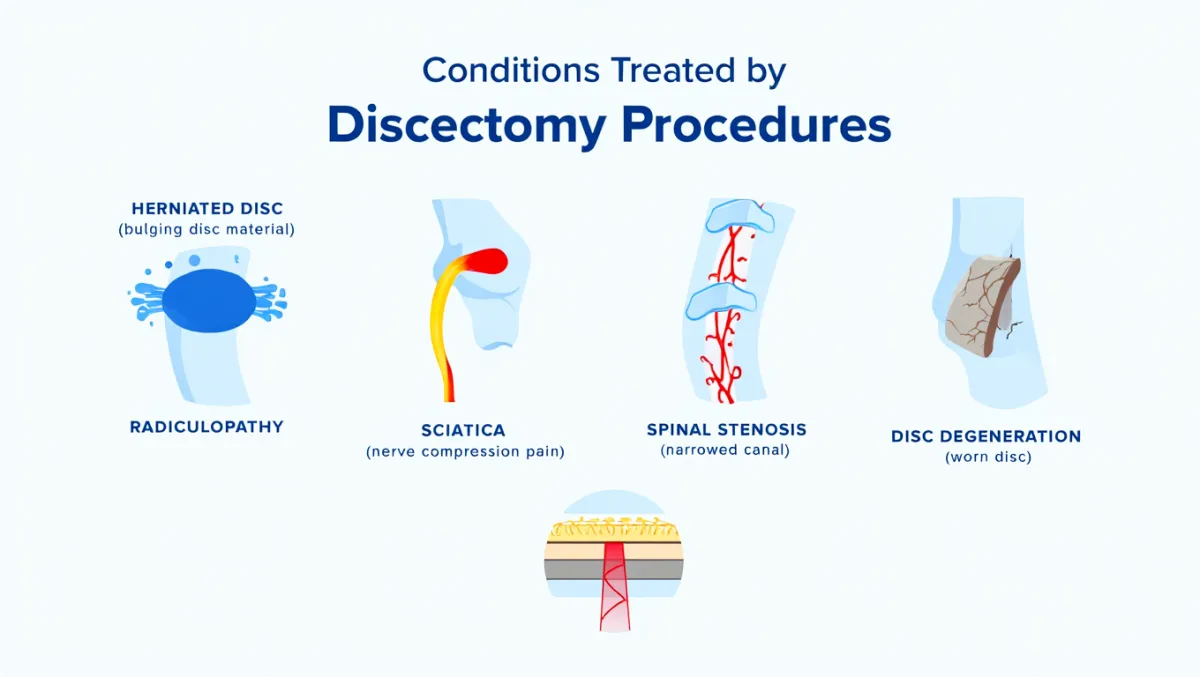
What Is a Discectomy?
In simple terms, we carefully remove the part of a herniated disc that is pressing on nerves, while leaving the healthy portion of the disc intact. Scientifically however, a discectomy involves annulotomy, nucleus fragment excision, and decompression of the neural elements, performed via microsurgical or endoscopic approaches through tubular retractors.
Spine Discectomy Procedures
Standard Discectomy
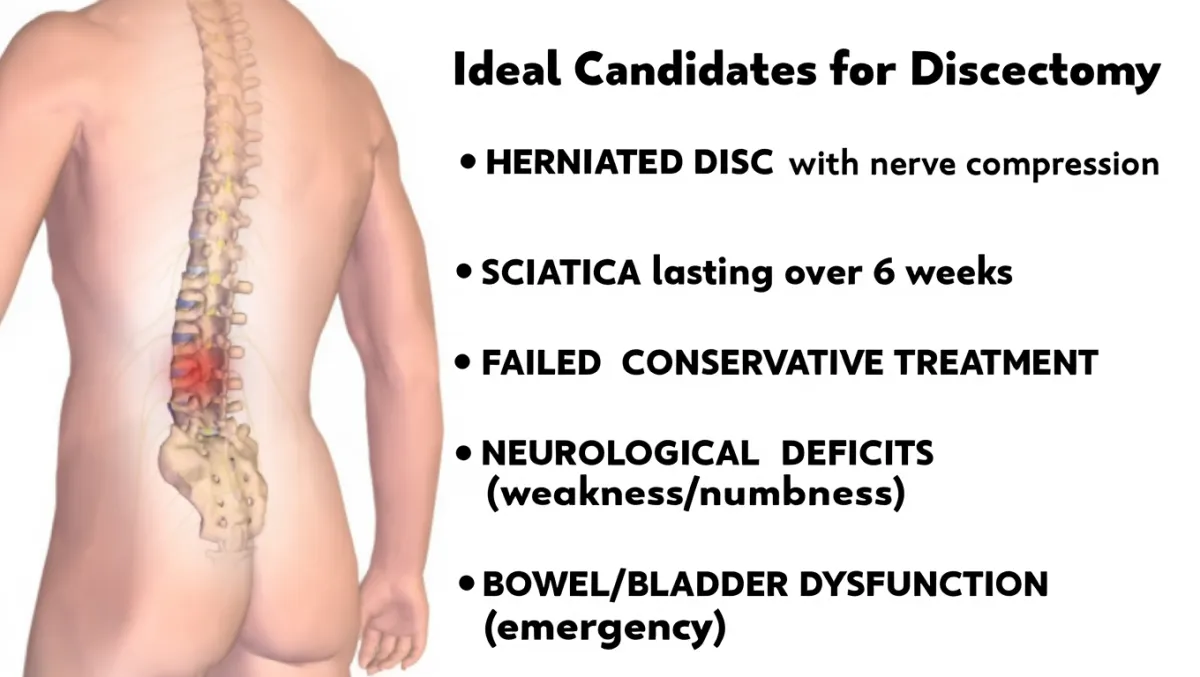
Standard Discectomy (also known simply as a lumbar discectomy) is a surgical procedure performed to remove a portion of a herniated or damaged disc that is pressing on nearby spinal nerves. When a disc bulges or ruptures, it can cause severe back pain, leg pain (sciatica), numbness, or weakness. The goal of the surgery is to relieve pressure on the nerves while preserving as much healthy disc tissue as possible.
During the procedure, Dr. David Greenwald makes a small incision in the back and gently moves aside muscles and soft tissue to access the spine. The part of the disc that is pressing on the nerve is carefully removed using microsurgical instruments, immediately relieving nerve compression. At Desert Spine and Pain, discectomy is often performed using microscopic or minimally invasive techniques, which reduce muscle disruption, minimize scarring, and promote quicker recovery. Most patients notice immediate relief of leg or arm pain, are able to walk the same day, and typically return home within 24 hours.
Lumbar Microdiscectomy
Lumbar Microdiscectomy is a minimally invasive spine surgery performed to relieve pressure on a nerve root in the lower back caused by a herniated or bulging disc. When a disc fragment compresses the spinal nerve, it can lead to sciatica—sharp, radiating leg pain, numbness, or weakness. This procedure is considered the gold standard for treating lumbar disc herniations that don’t improve with medications, therapy, or injections.
During the surgery, Dr. David Greenwald makes a small incision (typically less than one inch) in the lower back and uses a surgical microscope and microsurgical tools to remove only the portion of the disc pressing on the nerve—preserving the rest of the disc for stability. The minimally invasive approach used at Desert Spine and Pain means less tissue disruption, minimal blood loss, and faster recovery. Most patients walk within hours after surgery, go home the same day, and experience immediate relief of leg pain with a quick return to normal activity.
Anterior Cervical Discectomy Fusion (ACDF)
Anterior Cervical Discectomy and Fusion (ACDF) is one of the most common and effective surgeries used to treat herniated discs, bone spurs, or spinal cord compression in the neck. The procedure relieves pressure on the spinal cord and nerve roots—often caused by degenerative disc disease, cervical stenosis, or disc herniation—while stabilizing the affected vertebrae.
During ACDF, Dr. David Greenwald makes a small incision in the front of the neck (the anterior approach) to gently move aside muscles and soft tissue, providing direct access to the cervical spine. The damaged disc is carefully removed, relieving compression on the nerves and spinal cord. A bone graft or interbody cage is then placed in the empty disc space to maintain height and alignment, and a small plate with screws may be used for stability as the bones fuse together.
At Desert Spine and Pain, ACDF is performed using microsurgical and minimally invasive techniques to minimize discomfort and promote faster recovery. Most patients experience immediate improvement in arm pain and numbness, spend one night in the hospital or go home the same day, and return to light activity within a few weeks while the fusion heals fully over several months.
Anterior Cervical Discectomy with a Disc Replacement (ACDR)
Anterior Cervical Discectomy with Disc Replacement is a motion-preserving alternative to spinal fusion for patients with herniated cervical discs or degenerative disc disease in the neck. Like a traditional ACDF, this procedure relieves pressure on the spinal cord and nerves by removing the damaged disc—but instead of fusing the bones together, Dr. David Greenwald replaces the disc with an artificial implant that maintains natural motion between the vertebrae.
At Desert Spine and Pain, this advanced technique is performed through a small incision in the front of the neck (anterior approach) using microsurgical precision. After the diseased disc and any bone spurs are removed, the artificial disc is inserted to restore height, alignment, and flexibility. The implant functions much like a healthy disc—allowing bending and rotation while preventing future collapse or nerve compression. Patients benefit from less stiffness, faster recovery, and preserved neck movement compared to fusion. Most go home the same day and experience significant, lasting relief from arm pain, tingling, and weakness within weeks.
Book a Discectomy Consultation Today.
If you’re suffering from nerve pain or limited movement due to a herniated or bulging disc, a discectomy procedure may be the solution you need. Dr. Greenwald and his caring team will perform a thorough evaluation, explain your options, and determine the most effective treatment to relieve your pain and restore function. Every step you take toward treatment brings you closer to lasting relief and renewed confidence in your movement. Schedule your consultation today and let Dr. Greenwald help you regain comfort and quality of life through expert spinal care.


Dr. David L. Greenwald, M.D., F.A.C.S.
Neurosurgeon | Spine Surgeon | Regenerative Medicine
Dr. David L. Greenwald, MD, FACS, is a board-certified spine surgeon with advanced expertise in discectomy procedures, which are performed to remove the damaged portion of a herniated disc that is pressing on nearby spinal nerves. This targeted surgery is highly effective in relieving back or neck pain, as well as radiating leg or arm pain (sciatica or radiculopathy) caused by nerve compression. Dr. Greenwald specializes in both traditional and minimally invasive discectomy techniques, using small incisions and image-guided precision to minimize tissue disruption and promote faster recovery. His skill and patient-centered approach have helped countless individuals throughout South Florida experience long-term pain relief, improved mobility, and a return to active living.
The Discectomy Procedure: Step by Step
Here's how a discectomy procedure is performed, step by step - for both patients and in more technical terms along with some details on what you can expect from your recovery. Contact Desert Spine and Pain with questions.

Anesthesia & positioning
You’re asleep under general anesthesia, lying face down.

Incision
A small incision (often 1–2 cm) is made over the spine.

Muscle-sparing access
Muscles are gently separated using tubular retractors.

Microscope or endoscope
Provides magnified, illuminated view.

Bone window
A small portion of lamina and ligamentum flavum may be removed.

Disc removal
The herniated disc fragment is carefully removed.

Closure
The incision is closed; most patients walk the same day.
Discectomy Procedure Insights
Discectomy Surgical Procedure Steps
Docking: Fluoroscopy ensures exact level localization.
Laminotomy & flavectomy: Small opening made in lamina; ligamentum flavum partially removed.
Nerve root mobilization: Traversing/exiting root visualized and gently retracted.
Discectomy: Herniated nucleus pulposus fragment removed with pituitary rongeurs; annular defect inspected.
Hemostasis: Bipolar cautery; irrigation; tubular retractor removed.
Closure: Layered closure; sterile dressing applied.
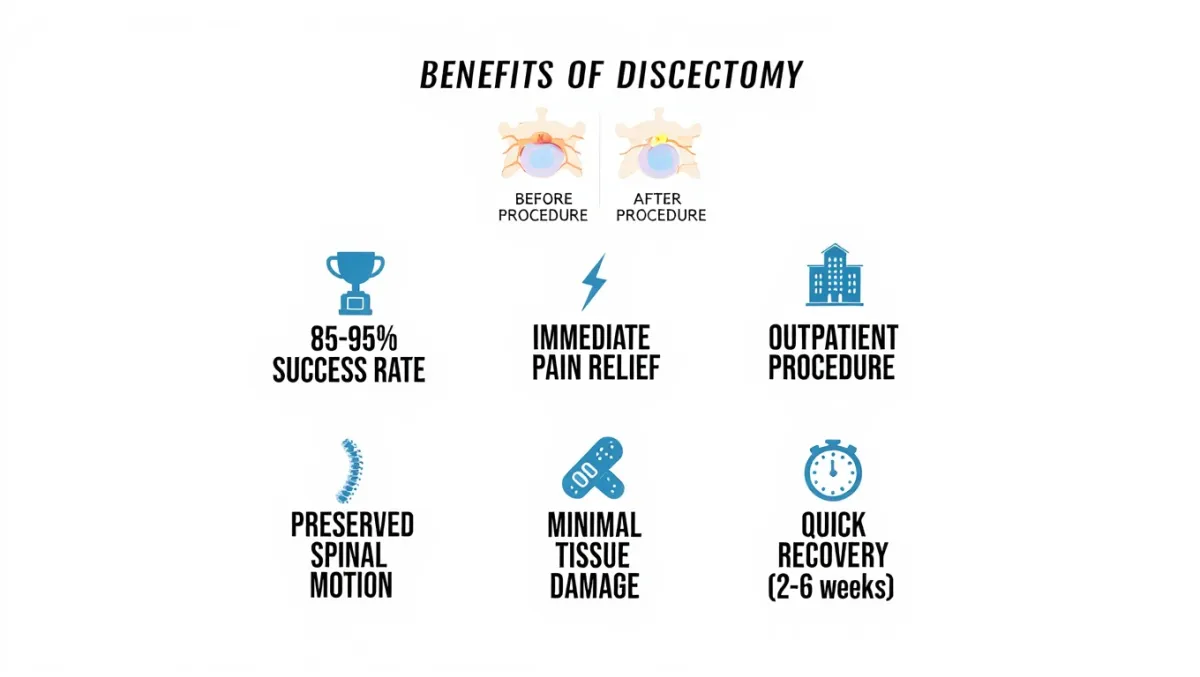
Benefits
Outpatient or overnight stay
Immediate relief of sciatica or nerve pain for most patients
Preserves stability (healthy disc left in place)
Tiny incision, minimal scarring
High success rates in well-selected patients
Risks & Limitations
Recurrence of herniated disc (5–15%)
Infection, bleeding, dural tear/CSF leak
Nerve root irritation or residual numbness
Does not “cure” degenerative disc disease; best for nerve compression symptoms
Why Choose Desert Spine and Pain?
Neurosurgeon-led care – Dr. Greenwald’s expertise ensures precision and safety
Minimally invasive focus – Smaller incisions, less muscle trauma, quicker recovery
Comprehensive care – Surgery only when conservative treatments fail
Compassionate guidance – We explain each step to reduce anxiety about surgery
Contact us today for a Spine and Pain Consultation. Relief is a phone call away!
Recovery Timeline

Day 0
Walk within hours; many go home same day

Weeks 1–2
Light activities, short walks daily

Weeks 2–6
Return to desk work; avoid bending/lifting/twisting

6–12 weeks
Resume most activities with PT guidance

3–6 months
Full nerve healing and strength return
Frequently Asked Questions
What’s the difference between microdiscectomy and endoscopic discectomy?
Both are minimally invasive. Microdiscectomy uses a microscope; endoscopic uses a camera. Choice depends on anatomy and surgeon preference.
Will a discectomy cure my back pain?
It’s most effective for leg or arm pain from nerve compression. Back pain may improve but is less predictable.
Can the disc herniate again?
Yes, in 5–15% of cases. If it does, revision surgery or fusion may be needed.
How long is the hospital stay?
Most patients go home the same day or after one night.
How does Desert Spine and Pain perform discectomy procedures differently?
We use the most minimally invasive, precise techniques available—always under the guidance of a neurosurgeon specializing in spine surgery.
Book your Spine Care Consultation Today!


Desert Spine and Pain
Patient Centered & Partner Focused
Quick Links
Resources
Connect With Us
© Desert Spine and Pain. 2026. All Rights Reserved. Sitemap