Discectomy Procedures
Anterior Cervical Discectomy with Disc Replacement (ACDR)
Preserving Motion in the Cervical Spine
An anterior cervical discectomy with disc replacement is a modern alternative to fusion. Instead of fusing two bones together after removing a damaged disc, the disc space is restored with an artificial disc implant that allows continued motion. At Desert Spine and Pain, neurosurgeon Dr. David L. Greenwald, M.D., FAANS, FACS carefully evaluates patients to determine whether disc replacement is the right choice. For the right patient, this procedure can relieve pain and pressure while maintaining neck mobility.

Over 100 5-Star Reviews!

What Is Cervical Disc Replacement?
In simple terms: We remove the damaged disc in the neck and replace it with a motion-preserving artificial disc instead of fusing the bones.
Scientifically: Cervical disc arthroplasty involves anterior cervical exposure, microsurgical discectomy, decompression of neural elements, and implantation of a mechanical prosthesis designed to replicate physiologic disc kinematics, preserving flexion, extension, lateral bending, and rotation.

Conditions Treated
Cervical radiculopathy from a herniated or degenerated disc
Cervical myelopathy (spinal cord compression, in select cases)
Degenerative disc disease at one or two levels
Patients who failed conservative treatments (PT, medications, injections)
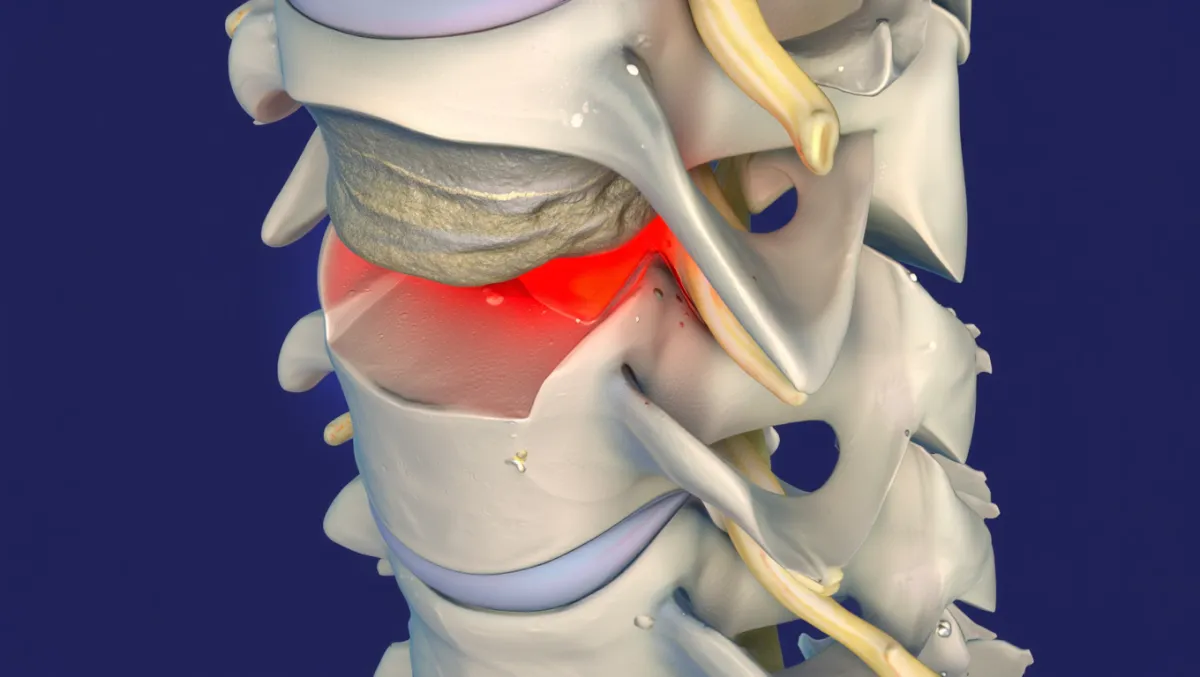
Who Is a Candidate?
Best candidates:
Younger, active patients
1–2 levels of disc disease
No severe arthritis or deformity
No instability or need for multi-level fusion
Not ideal for:
Severe spondylosis/arthritis
Spinal instability or deformity
Osteoporosis
Multi-level disease beyond 2 levels
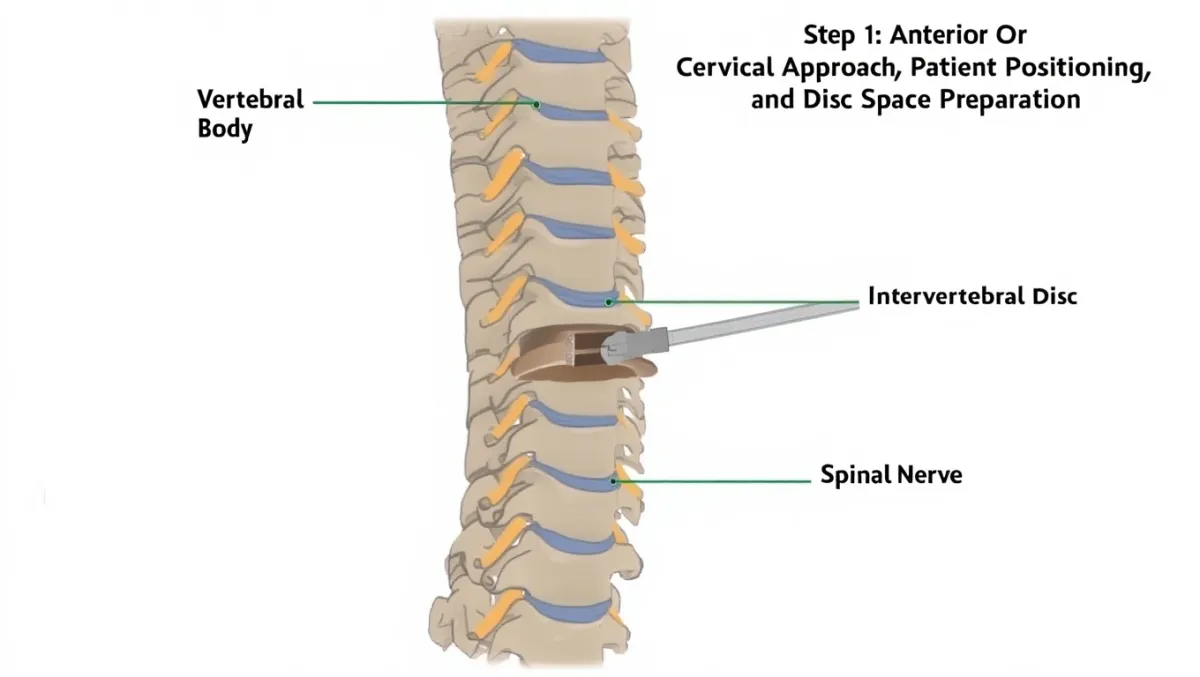
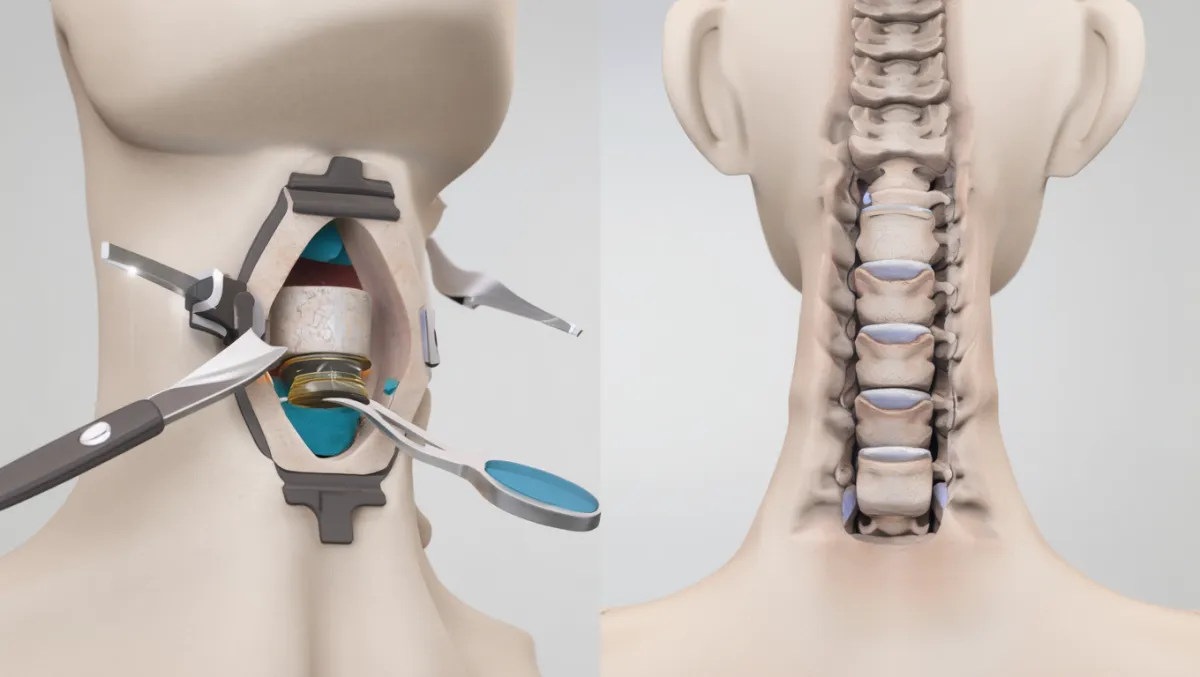
The Disc Replacement Procedure: Step by Step
Plain-English Overview
Anesthesia & positioning: You’re asleep under general anesthesia, lying on your back.
Small incision: A 1–2 inch incision is made in the front of the neck.
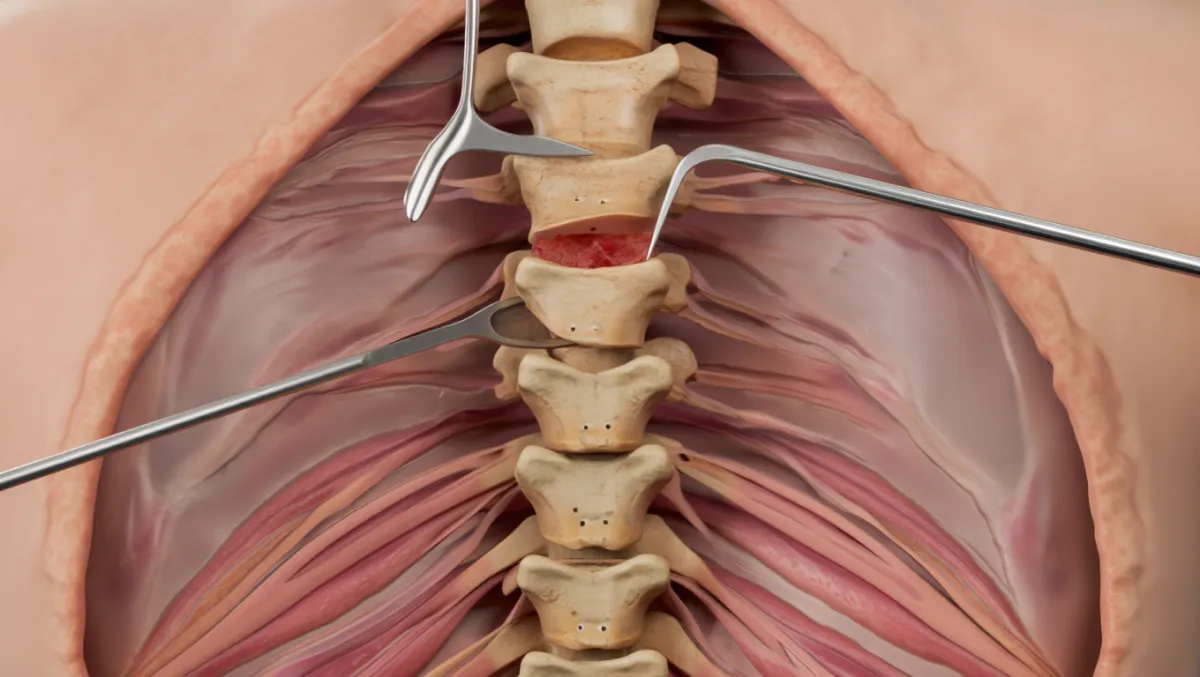
Disc removal: The damaged disc and bone spurs are removed.
Nerve decompression: Spinal cord and nerve roots are freed.
Artificial disc placement: An artificial disc is placed in the disc space, restoring motion.
Closure: The incision is closed; patients often walk the same day.
Surgeon-Level Detail
Exposure: Smith-Robinson anterior approach with blunt dissection to prevertebral fascia.
Localization: Fluoroscopy ensures correct level.
Discectomy: Microsurgical annulotomy, nucleus removal, posterior longitudinal ligament resection as needed.
Decompression: Osteophyte removal with drill/Kerrisons; confirm free neural elements.
Disc replacement: Endplates prepared precisely; trialing performed; prosthesis (metal/polymer or metal-on-metal design) implanted under fluoroscopy.
Closure: Irrigation; layered closure with absorbable sutures; drain rarely needed.
Benefits of Disc Replacement
Preserves motion at the treated level
Reduces stress on adjacent discs (lower risk of adjacent segment disease compared to fusion)
Small incision, outpatient or 1-night stay
Reliable relief of arm pain, numbness, and weakness
Faster return to activity than fusion in many cases
Risks & Limitations
Difficulty swallowing (temporary dysphagia)
Hoarseness (recurrent laryngeal nerve irritation)
Implant-related complications (migration, wear, or mechanical failure—rare)
Not suitable for severe arthritis or instability
Fusion may still be required in some cases if disc replacement fails
Recovery Timeline
Day 0: Walking same day; many patients go home within 24 hours
Weeks 1–2: Mild neck/throat soreness; gradual return to light activity
Weeks 2–6: Desk work and driving usually resumed
6–12 weeks: Begin structured physical therapy for strength and posture
3–6 months: Full activity for most patients; disc mobility preserved
12 months: Continued monitoring with X-rays to confirm implant position

Why Choose Desert Spine and Pain?
Motion-preservation expertise: Dr. Greenwald is highly trained in both fusion and artificial disc replacement
Conservative-first philosophy: Surgery only when conservative options fail
Personalized care: Careful evaluation to decide between ACDF and disc replacement
Advanced technology: State-of-the-art implants and precision microsurgery
Frequently Asked Questions
How is disc replacement different from ACDF?
Disc replacement preserves motion at the treated level, while ACDF fuses the bones together. Both relieve nerve compression effectively.
Is disc replacement safe?
Yes. Complications are rare, and implants are FDA-approved and studied extensively.
Will I lose motion in my neck?
No. The artificial disc is designed to preserve normal motion.
How long does a disc replacement last?
Studies suggest durability for 10–20+ years, but long-term data is still evolving.
How does Desert Spine and Pain approach disc replacement differently?
We carefully select patients who will truly benefit, ensuring the safest, most effective outcome while avoiding unnecessary fusion.




Dr. David L. Greenwald, MD
Neuro-Spine Surgeon

Call Now!
Desert Spine and Pain
A Spine Specialist is standing by.
Relief is just a phone call away!
Available Around the Clock.
Phone: (602) 566-9500
Email: [email protected]
Contact Us

Book a Consultation.
If you’re suffering from neck pain, arm weakness, or nerve symptoms caused by a herniated or degenerated cervical disc, Anterior Cervical Discectomy with Disc Replacement (ACDR) may be the ideal solution. Dr. Greenwald and his caring team will evaluate your condition, review imaging, and determine if ACDR is right for you. Every step you take toward advanced spine care brings you closer to comfort, flexibility, and a better quality of life. Schedule your consultation today and discover how Dr. Greenwald’s expertise in motion-preserving surgery can help you move freely and live pain-free.

Voted Best Spine Doctor
Over 30 Years Experience in Orthopedic & Neuro Spine Surgeries.

Dr. David L. Greenwald, M.D., F.A.C.S.
Neurosurgeon | Spine Surgeon | Regenerative Medicine
Dr. David L. Greenwald, MD, FACS, is a board-certified spine surgeon with advanced expertise in Anterior Cervical Discectomy with Disc Replacement (ACDR), a motion-preserving procedure that relieves pressure on the spinal cord or nerves while maintaining natural neck movement. During this minimally invasive surgery, Dr. Greenwald removes the damaged cervical disc through a small incision in the front of the neck and replaces it with a high-performance artificial disc designed to mimic the function of a healthy one. ACDR is often recommended for patients with cervical disc herniation, degenerative disc disease, or nerve compression. Dr. Greenwald’s precision and experience allow patients throughout South Florida to experience significant pain relief, restored function, and faster recovery without sacrificing mobility.
Book your Spine Care Consultation Today!


Desert Spine and Pain
Patient Centered & Partner Focused
Quick Links
Resources
Connect With Us
© Desert Spine and Pain. 2026. All Rights Reserved. Sitemap