Decompression
Corpectomy
Advanced Decompression for Severe Spinal Cord Compression
A corpectomy is a surgical procedure where part or all of a vertebral body and adjacent discs are removed to decompress the spinal cord and nerves. This is typically performed for severe stenosis, tumors, fractures, or deformities that cannot be treated with simpler procedures like laminectomy or discectomy. At Desert Spine and Pain, neurosurgeon Dr. David L. Greenwald, M.D., FAANS, FACS performs corpectomies using advanced techniques to relieve spinal cord pressure, reconstruct stability, and restore alignment.

Over 100 5-Star Reviews!


What Is a Corpectomy?
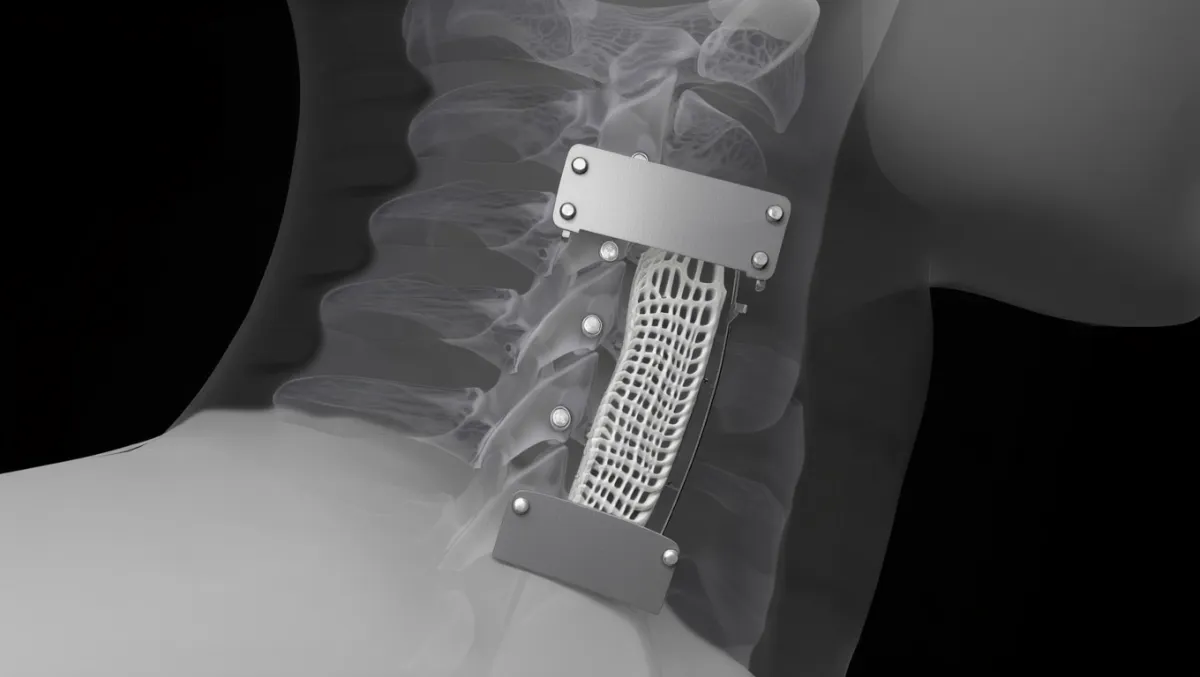
In simple terms: A corpectomy removes part of the spinal bone and discs above and below it to take pressure off the spinal cord and nerves. The area is then rebuilt with a cage and bone graft to stabilize the spine.
Scientifically: Corpectomy (vertebrectomy) involves en bloc removal of vertebral body segments and adjacent intervertebral discs, followed by reconstruction with titanium mesh cage, expandable cage, or allograft strut plus anterior/posterior instrumentation.

Conditions Treated
Severe spinal stenosis with cord compression
Cervical myelopathy or thoracic myelopathy
Vertebral body fractures from trauma or osteoporosis
Spinal tumors involving vertebral body
Kyphosis or deformity requiring correction
Failed prior surgeries with persistent compression

The Corpectomy Procedure: Step by Step
Plain-English Overview
Anesthesia & positioning: You’re asleep under general anesthesia. Approach may be from the front (anterior) or back (posterior) depending on location.
Incision: Made in the neck, chest, abdomen, or back depending on spinal region.
Vertebral body removal: The diseased bone and adjacent discs are carefully removed.
Decompression: The spinal cord and nerves are freed from compression.
Reconstruction: A cage or graft filled with bone is inserted to restore height.
Stabilization: Plates, screws, or rods are placed to secure the spine.
Closure: Incision is closed; patients usually stay in the hospital a few days.
Surgeon-Level Detail
Exposure:
Cervical: Smith-Robinson anterior approach.
Thoracic: Transthoracic or lateral extracavitary.
Lumbar: Retroperitoneal or posterior transpedicular.
Decompression: Removal of vertebral body with drill/rongeurs; resection of PLL, osteophytes, tumor, or fragments compressing cord.
Reconstruction: Expandable cage or mesh cage packed with autograft/allograft; endplate preparation essential.
Fixation: Anterior plating or posterior pedicle screw/rod constructs for immediate stability.
Fusion biology: Autograft (iliac crest), allograft, BMP, or synthetic substitutes used.

Benefits of Corpectomy
Provides direct and wide decompression of the spinal cord
Corrects deformity and restores spinal alignment
Allows removal of tumors or fractures not manageable otherwise
When combined with fusion, provides strong long-term stability
Risks & Limitations
More invasive than discectomy or laminectomy
Higher blood loss and longer operative time
Risks: infection, bleeding, CSF leak, graft/implant failure, non-union
Neurological complications possible given severity of disease
Longer recovery compared to smaller decompressions
Recovery Timeline
Hospital stay: Typically 2–5 days depending on region/complexity
Weeks 1–2: Wound care, light walking; brace may be prescribed
Weeks 2–6: Gradual increase in activity; desk work possible
6–12 weeks: Begin structured physical therapy; restrictions eased gradually
3–6 months: Fusion consolidating; improved strength and stability
6–12 months: Full recovery with stable fusion on imaging
Why Choose Desert Spine and Pain?
Expert neurosurgeon: Dr. Greenwald has decades of experience performing complex corpectomies safely
Advanced reconstruction tools: Expandable cages, navigation, and microsurgical techniques
Comprehensive care: From diagnosis to rehab, everything under one roof
Patient-centered approach: We guide you through the process, easing fears about such a major surgery

Frequently Asked Questions
Why would I need a corpectomy instead of a discectomy?
Corpectomy is chosen when compression extends beyond a single disc space, involves bone, or requires wider decompression.
How invasive is a corpectomy?
It’s more invasive than standard decompression, but often the best or only way to fully relieve spinal cord compression.
Will I need a fusion after a corpectomy?
Yes. Fusion and stabilization are always performed after vertebral body removal.
How long before I recover?
Most patients notice improved nerve function within weeks, but full recovery—including fusion—takes 6–12 months.
How does Desert Spine and Pain perform corpectomy differently?
We use neurosurgical precision, advanced implants, and minimally invasive exposures whenever possible to maximize safety and recovery.




Dr. David L. Greenwald, MD
Neuro-Spine Surgeon

Call Now!
Desert Spine and Pain
A Spine Specialist is standing by.
Relief is just a phone call away!
Available Around the Clock.
Phone: (602) 566-9500
Email: [email protected]
Contact Us

Book a Consultation.
If you’ve been diagnosed with a condition requiring spinal decompression or reconstruction, a corpectomy may be the right treatment to relieve pressure and restore spinal stability. Dr. Greenwald and his compassionate team will thoroughly evaluate your imaging, explain your options, and create a surgical plan tailored to your needs. Every step you take toward expert spine care brings you closer to comfort, mobility, and confidence. Schedule your consultation today and learn how Dr. Greenwald’s skill in corpectomy surgery can help you achieve long-term relief and spinal health.

Voted Best Spine Doctor
Over 30 Years Experience in Orthopedic & Neuro Spine Surgeries.

Dr. David L. Greenwald, M.D., F.A.C.S.
Neurosurgeon | Spine Surgeon | Regenerative Medicine
Dr. David L. Greenwald, MD, FACS, is a board-certified spine surgeon with extensive experience performing corpectomy procedures to relieve spinal cord or nerve compression caused by trauma, tumors, or severe degenerative conditions. A corpectomy involves removing part or all of a vertebral body and adjacent discs to decompress the spinal cord and restore stability to the spine. Dr. Greenwald utilizes advanced imaging and minimally invasive or microsurgical techniques to ensure precision, reduce recovery time, and promote long-term spinal alignment. His expertise allows patients throughout South Florida to experience meaningful pain relief, improved neurological function, and a restored quality of life after complex spinal conditions.
Book your Spine Care Consultation Today!


Desert Spine and Pain
Patient Centered & Partner Focused
Quick Links
Resources
Connect With Us
© Desert Spine and Pain. 2026. All Rights Reserved. Sitemap
