Minimally Invasive Surgery
MIS Sacroiliac Fusion (SI Fusion)
Stabilizing the Joint Between Spine and Pelvis
The sacroiliac (SI) joint connects the spine to the pelvis. When this joint becomes unstable or arthritic, it can cause severe low back, buttock, or leg pain that often mimics other spine conditions. If conservative treatments fail, a sacroiliac fusion (SI fusion) may be recommended to stabilize the joint and provide lasting pain relief. At Desert Spine and Pain, Dr. David L. Greenwald, M.D., FAANS, FACS, a nationally recognized neurosurgeon, performs SI fusion using minimally invasive techniques designed for smaller incisions, less pain, and quicker recovery.

Over 100 5-Star Reviews!


What Is Sacroiliac Fusion?
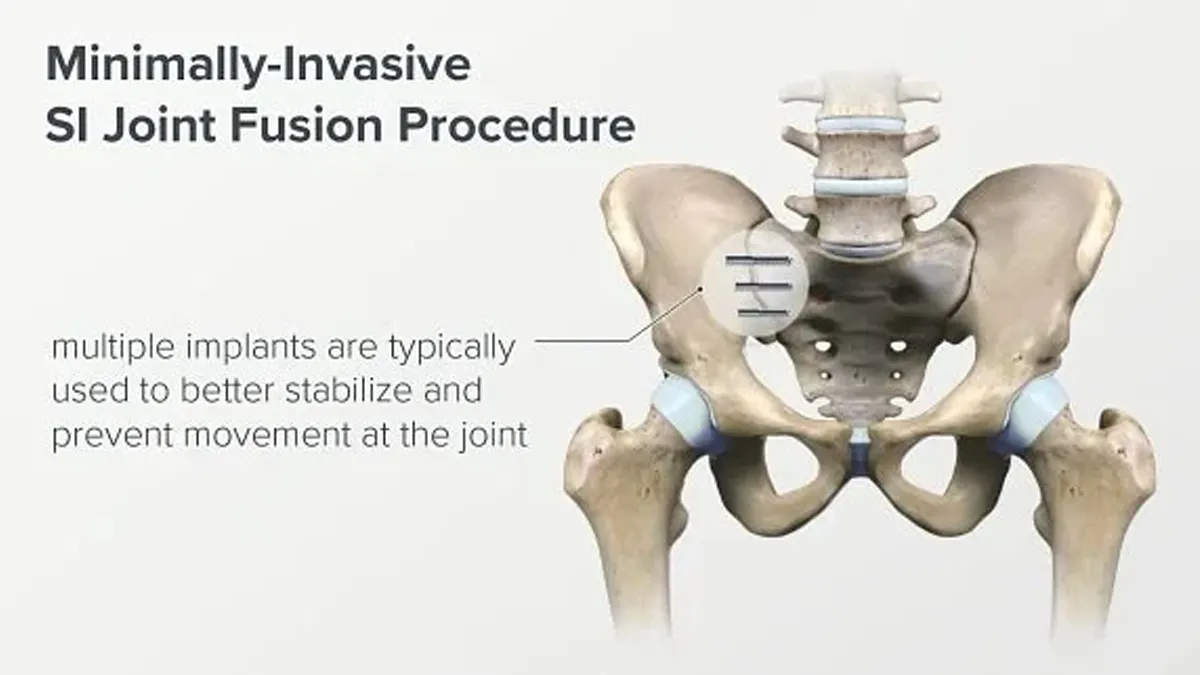
In simple terms: SI fusion joins the sacrum (base of the spine) and ilium (pelvic bone) together using implants so the painful joint no longer moves.
Scientifically: SI fusion involves percutaneous placement of implants (typically titanium or 3D-printed porous devices) across the SI joint under fluoroscopic guidance, promoting bony arthrodesis and eliminating pathological micromotion.

Conditions Treated
Sacroiliac joint dysfunction causing chronic low back and buttock pain
Sacroiliac degeneration from arthritis or wear and tear
SI joint instability after trauma, pregnancy, or spine surgery (e.g., after fusion extending to the sacrum)
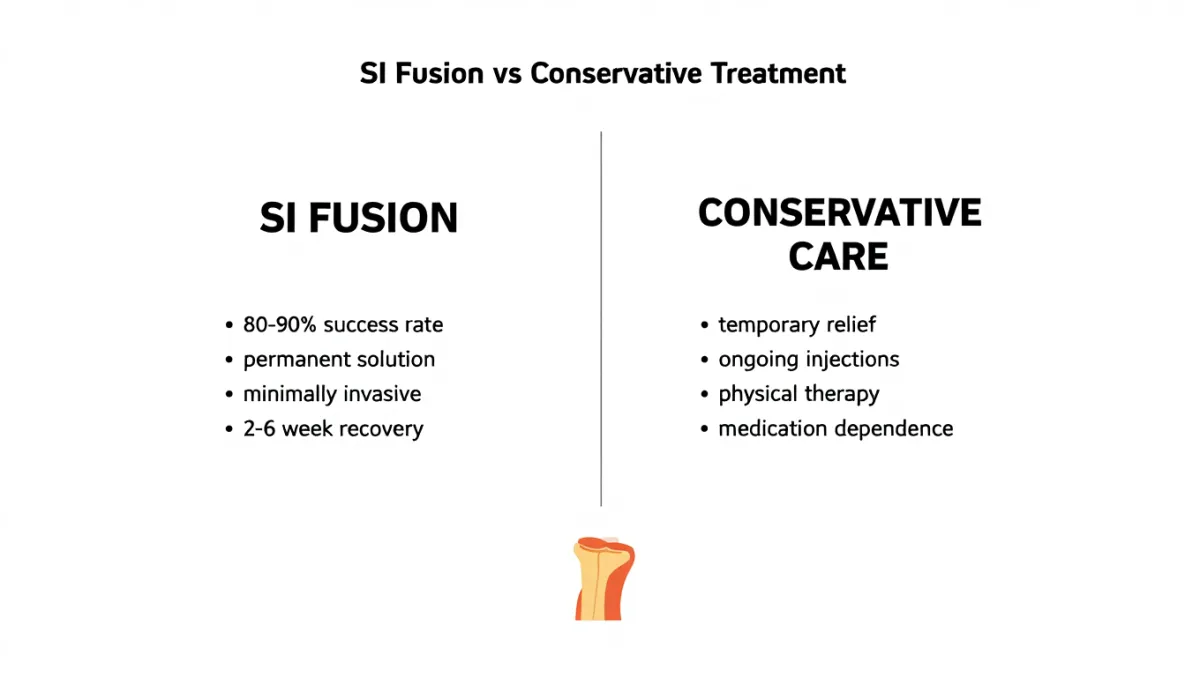
Failed conservative treatment (PT, injections, bracing)
Pre-Operative Workup
History & exam: SI joint provocative maneuvers (e.g., FABER test)
Imaging: X-ray, CT, MRI to confirm SI degeneration and rule out lumbar spine issues
Diagnostic injection: Pain relief after SI joint injection confirms diagnosis before fusion
Optimization: PT, medications, and bracing are tried first; surgery only if pain persists
The SI Fusion Procedure: Step by Step
Plain-English overview
Anesthesia & positioning: You’re asleep (general anesthesia), lying face down.
Small incision: A 2–3 cm incision is made along the buttock.
Guided implant placement: Using live X-ray (fluoroscopy), instruments are passed across the SI joint.
Joint stabilization: 2–3 implants are placed to secure the joint.
Closure: Incision closed with sutures or glue; many patients go home the same day.
Surgeon-level detail
Approach: MIS lateral buttock incision; dissection to lateral ilium under fluoroscopic control.
Trajectory: Guide pins advanced across ilium into sacrum; confirm with AP/inlet/outlet views.
Preparation: Drilling/burring across SI joint, decortication of bone to promote fusion.
Implant insertion: 2–3 triangular titanium or porous-coated implants placed across joint; position confirmed with multiple fluoro angles.
Fixation: Immediate stability achieved; long-term fusion occurs as bone grows through implants.
Closure: Layered closure; sterile dressing.
Benefits of SI Fusion
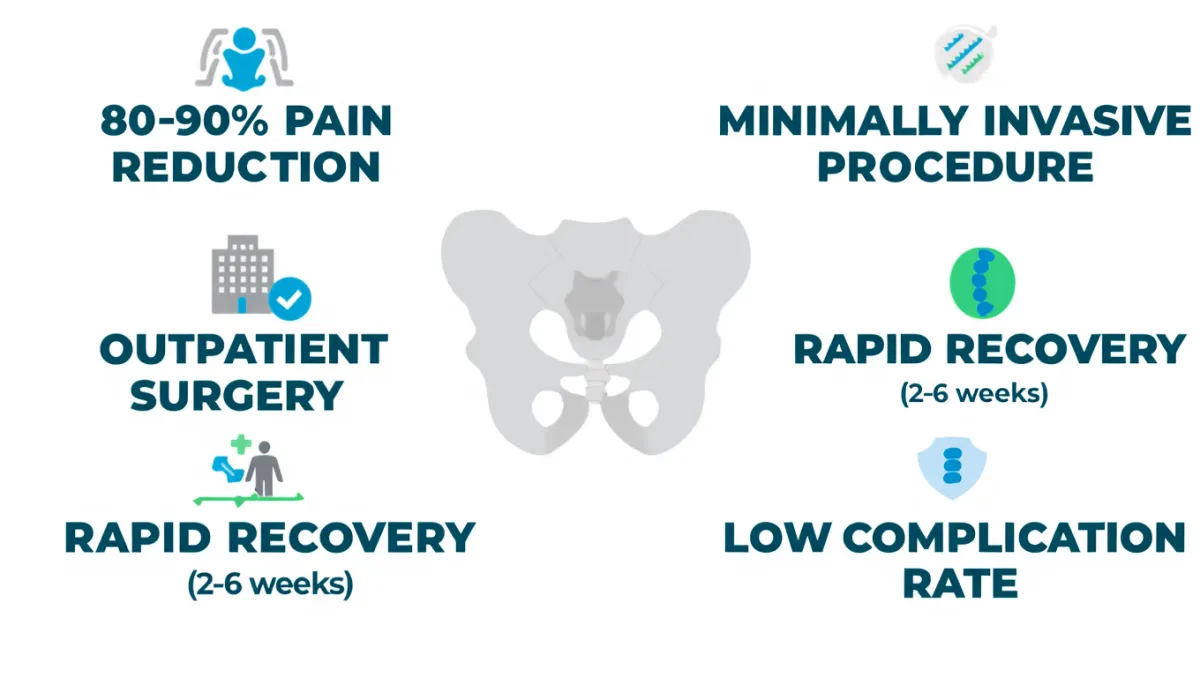
Minimally invasive; outpatient in most cases
Small incision with low blood loss
Faster recovery compared to open SI joint fusion
Provides permanent stabilization for painful SI dysfunction
High success rates in properly selected patients
Risks & Limitations
Infection, bleeding, implant malposition
Nerve irritation (rare, minimized by careful fluoroscopic guidance)
Non-union (failure to fuse)
Persistent pain if other pain generators present (lumbar spine, hip, etc.)
Not appropriate if pain isn’t truly from the SI joint (diagnostic injections are key)
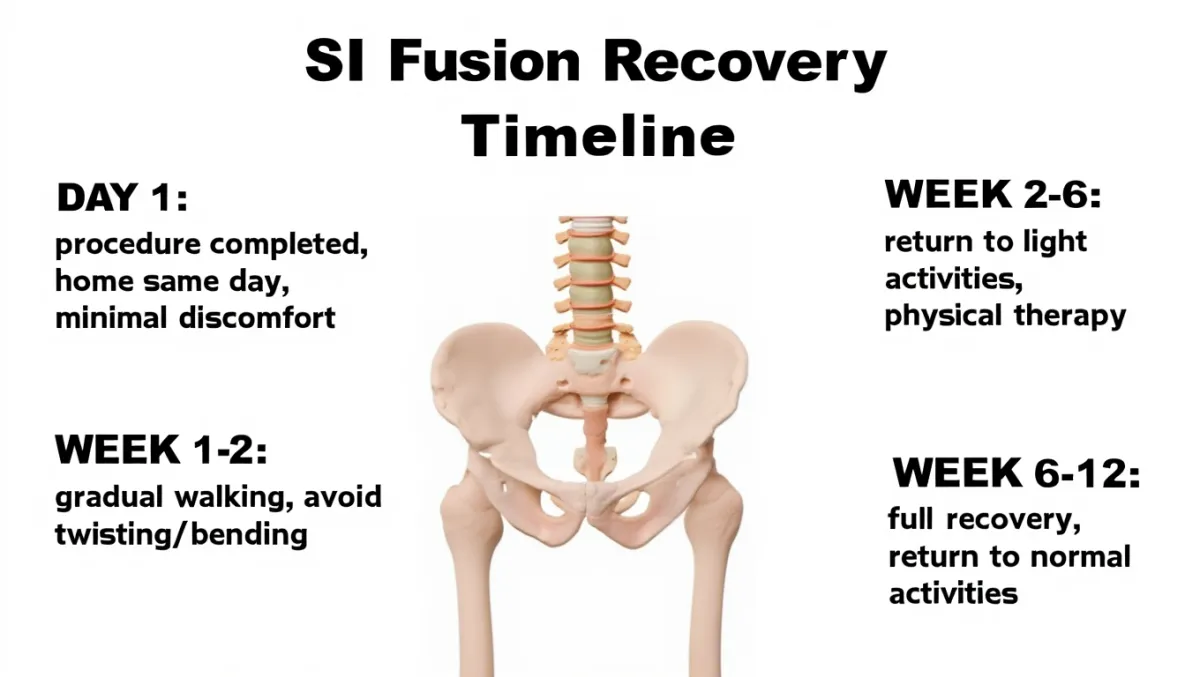
Recovery Timeline
Day of surgery: Walking the same day; discharged home
Week 1–2: Mild soreness; light activity encouraged
Weeks 2–6: Gradual return to daily activities; restrictions on heavy lifting/twisting
6–12 weeks: Fusion maturing; physical therapy may begin
3–6 months: Most patients resume full activity with long-term pain relief
Why Choose Desert Spine and Pain?
Expert neurosurgeon: Dr. Greenwald is skilled in minimally invasive SI fusion techniques
Comprehensive care: Diagnostic injections, PT, and conservative care are always attempted first
Patient-first approach: Surgery only when it’s truly necessary and beneficial
Advanced technology: Image-guided implant placement for maximum safety and accuracy
Frequently Asked Questions
How do I know if my pain is from the SI joint?
A diagnostic injection that relieves your pain confirms the joint as the source.
Will SI fusion cure my back pain?
If your pain truly comes from the SI joint, fusion can provide long-term relief. If pain is from another source, results may vary.
How long until I feel better?
Many patients notice improvement within weeks, with maximum benefit by 3–6 months.
Will I lose mobility after SI fusion?
No. The SI joint has very limited motion normally, so fusion does not affect flexibility.
How does Desert Spine and Pain perform SI fusion differently?
We combine neurosurgical precision, advanced implants, and careful patient selection to maximize safety and outcomes.




Dr. David L. Greenwald, MD
Neuro-Spine Surgeon

Call Now!
Desert Spine and Pain
A Spine Specialist is standing by.
Relief is just a phone call away!
Available Around the Clock.
Phone: (602) 566-9500
Email: [email protected]
Contact Us

Schedule a Consultation Now.
If you’re struggling with chronic lower back or pelvic pain that hasn’t improved with conservative treatments, Sacroiliac Fusion (SI Fusion) may be an effective solution. Dr. Greenwald and his compassionate team will thoroughly evaluate your condition, explain your treatment options, and determine whether SI Fusion is right for you. Every step you take toward expert spine care brings you closer to relief, stability, and restored movement. Schedule your consultation today and discover how Dr. Greenwald can help you regain comfort and confidence in your daily life.

Voted Best Spine Doctor
Over 30 Years Experience in Orthopedic & Neuro Spine Surgeries.

Dr. David L. Greenwald, M.D., F.A.C.S.
Neurosurgeon | Spine Surgeon | Regenerative Medicine
Dr. David L. Greenwald, MD, FACS, is a board-certified spine surgeon with advanced expertise in Sacroiliac Fusion (SI Fusion), a minimally invasive surgical procedure used to treat chronic pain originating from the sacroiliac (SI) joint. When the SI joint becomes unstable or degenerative, it can cause persistent lower back, hip, or pelvic pain. Dr. Greenwald uses image-guided technology and small incisions to stabilize the joint with precision, reducing pain while preserving surrounding muscles and tissues. His patient-centered approach and surgical expertise allow individuals throughout South Florida to experience faster recovery, improved function, and long-term pain relief after SI joint fusion.
Book your Spine Care Consultation Today!


Desert Spine and Pain
Patient Centered & Partner Focused
Quick Links
Resources
Connect With Us
© Desert Spine and Pain. 2026. All Rights Reserved. Sitemap