Minimally Invasive Surgery
Interlaminar Lumbar Interbody Fusion (ILIF)
A side-approach, minimally invasive lumbar fusion
At Desert Spine and Pain, Extreme Lateral Interbody Fusion (XLIF) is one of our advanced minimally invasive options for stabilizing the lower spine and relieving pinched nerves when conservative care hasn’t been enough. Led by Dr. David L. Greenwald, M.D., FAANS, FACS—a nationally recognized neurosurgeon—we perform XLIF through a small side (lateral) incision, sparing back muscles and typically speeding recovery.

Over 100 5-Star Reviews!

What ILIF Is (two ways to understand it)
In simple terms: Through a small back incision, we create space between two backbones, remove the painful disc, place a cage with bone graft, and add screws/rods to stabilize so the bones grow together.
Scientifically: Using a midline or paramedian MIS posterior approach, we perform a limited laminotomy/interlaminar decompression and partial facetectomy to access the disc. After discectomy and endplate preparation, a lordotic interbody cage with graft is inserted across the disc space. Percutaneous pedicle screws provide posterior fixation. This offers direct decompression plus interbody stabilization—similar goals to MIS TLIF, but via the interlaminar corridor.
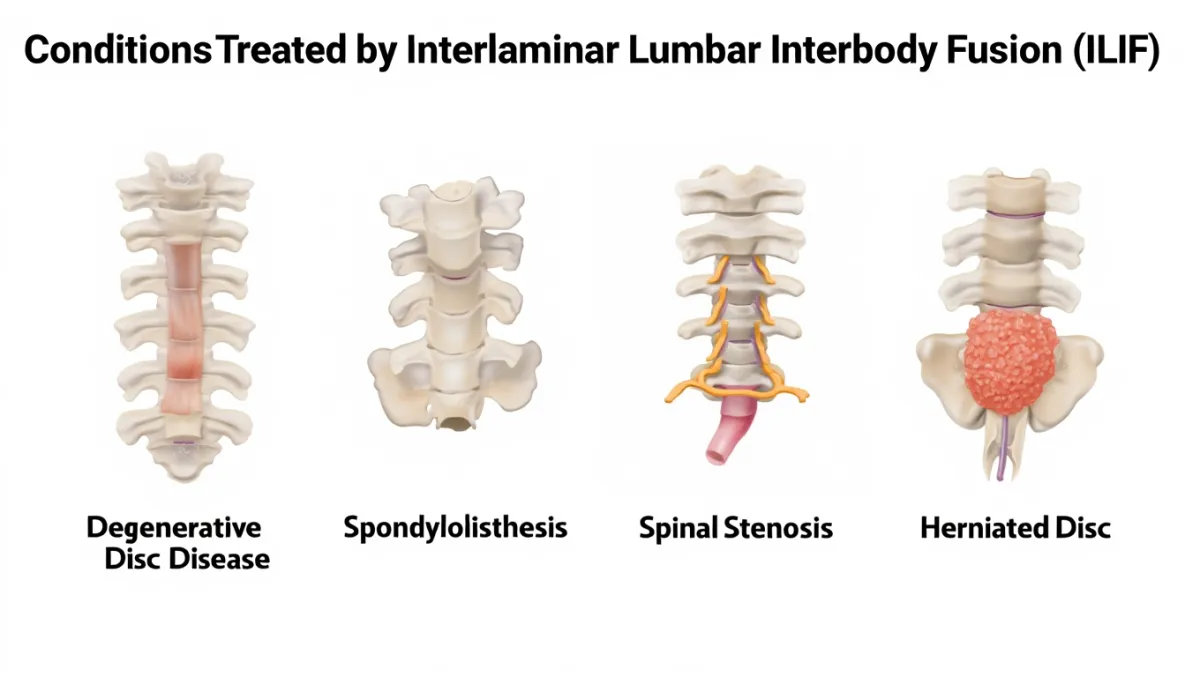
Indications (when we use ILIF)
Unilateral or bilateral radiculopathy with foraminal/central stenosis needing direct posterior decompression
Degenerative spondylolisthesis (low–moderate) with instability or recurrent symptoms
Degenerative disc disease with mechanical back pain and nerve compression
When lateral access (XLIF) isn’t favorable due to anatomy or prior surgery
Pre-Op Planning
MRI/CT to assess laminar width, facet hypertrophy, and foraminal stenosis
Standing radiographs for alignment and slip grade
Medical optimization (nicotine cessation, bone health) and prehab PT

The ILIF Procedure: Full Walkthrough
Plain-English overview
Anesthesia & positioning: You’re asleep and lie on your stomach; we pad all pressure points.
Small midline/paramedian incision: We gently split muscles to the back of the spine—no large muscle stripping.
Interlaminar window: We remove a small portion of bone/ligament to open the canal and free the pinched nerve(s).
Disc removal: We reach the disc through the opened window, remove the damaged disc, and clean the bone surfaces.
Cage with bone graft: We place a cage filled with graft to restore disc height and create the bridge for fusion.
Screws/rods: Through tiny incisions, percutaneous pedicle screws add stability.
Close & recover: Many patients walk the same day or next morning.
Surgeon-level detail
Approach: MIS midline split or Wiltse paramedian approach with tubular retractor; fluoroscopic level confirmation.
Decompression: Hemi laminotomy/laminotomy ± medial facetectomy; ligamentum flavum removal; direct visualization of traversing/exiting roots; foraminotomy as needed.
Disc work: Annulotomy; meticulous discectomy; endplate preparation preserving cortical shell to reduce subsidence.
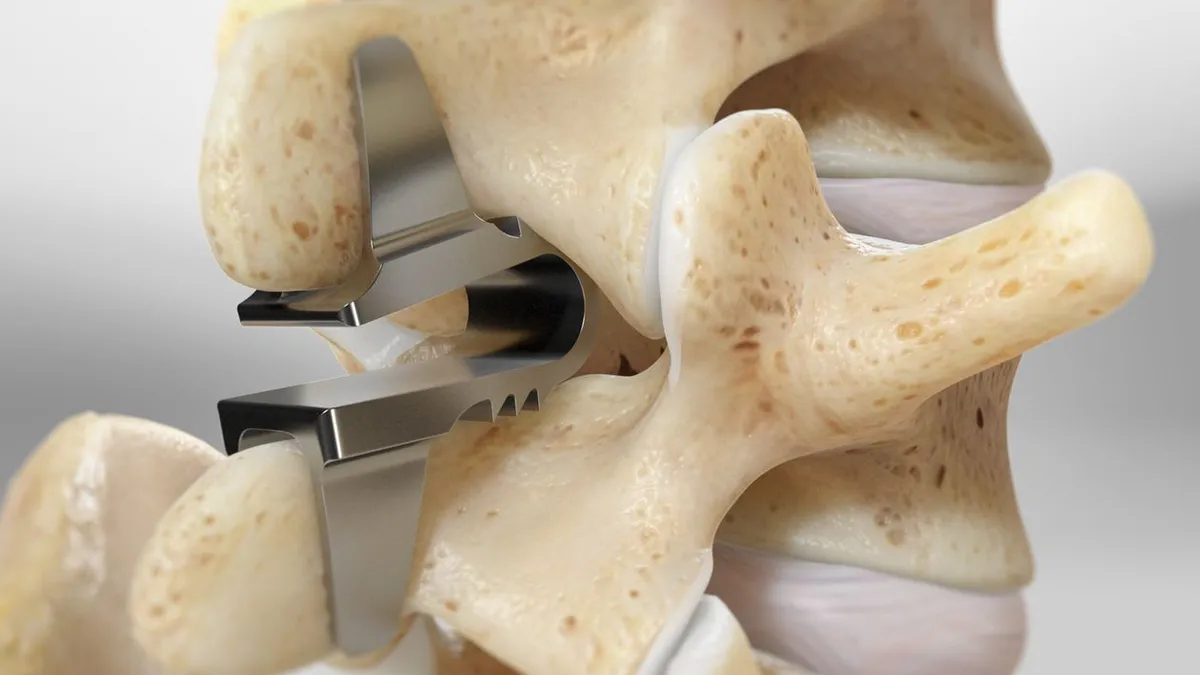
Interbody cage: Trial sizing; insert lordotic cage (PEEK/titanium) with autograft/allograft to restore height and foraminal area.
Fixation: Bilateral percutaneous pedicle screws/rods; reduction maneuvers if spondylolisthesis.
Imaging/closure: Fluoro confirms placement; layered closure; drains seldom needed.
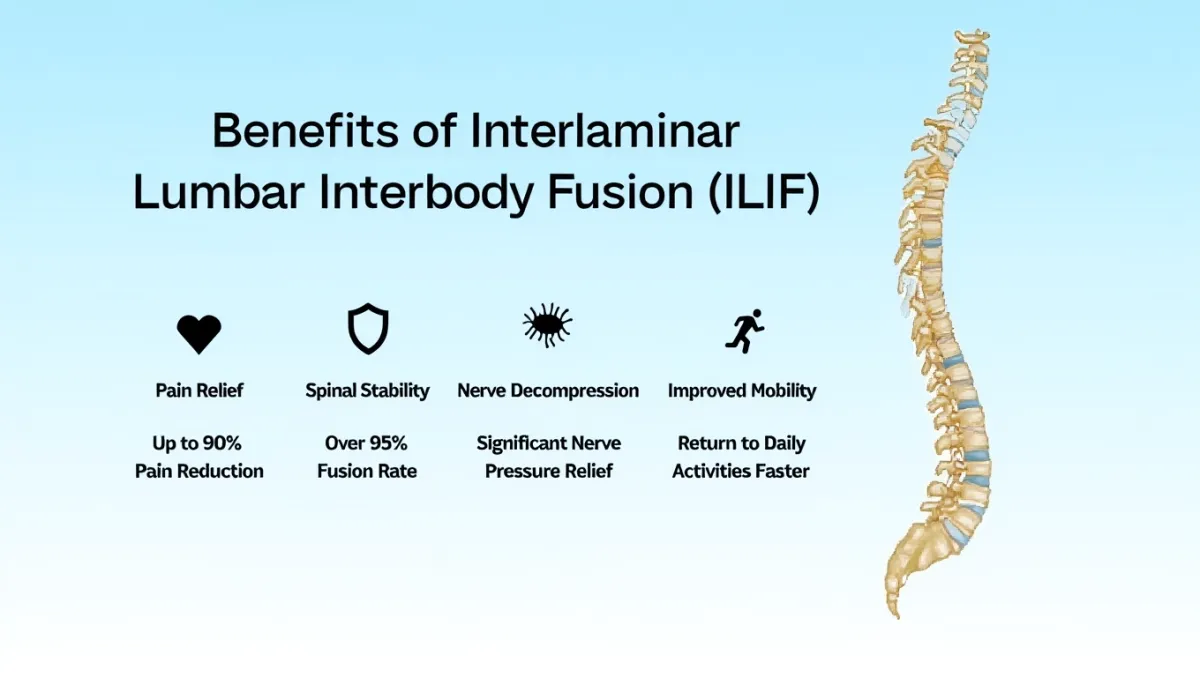
Benefits of ILIF
Direct decompression of nerve roots (ideal when stenosis is tight)
Muscle-sparing posterior approach with small incisions
Stable fusion with percutaneous screws
Works well at L4–5 and L5–S1, including cases where lateral access is blocked by the iliac crest
Risks & Mitigation
Dural tear/CSF leak — minimized by microsurgical technique; repaired immediately if encountered
Nerve root irritation/weakness — mitigated by careful root handling and neuromonitoring
Infection, bleeding, non-union, hardware issues — reduced via sterile technique, antibiotics, fixation accuracy, and fusion-supportive aftercare
DVT/PE — early ambulation and risk-based prophylaxis
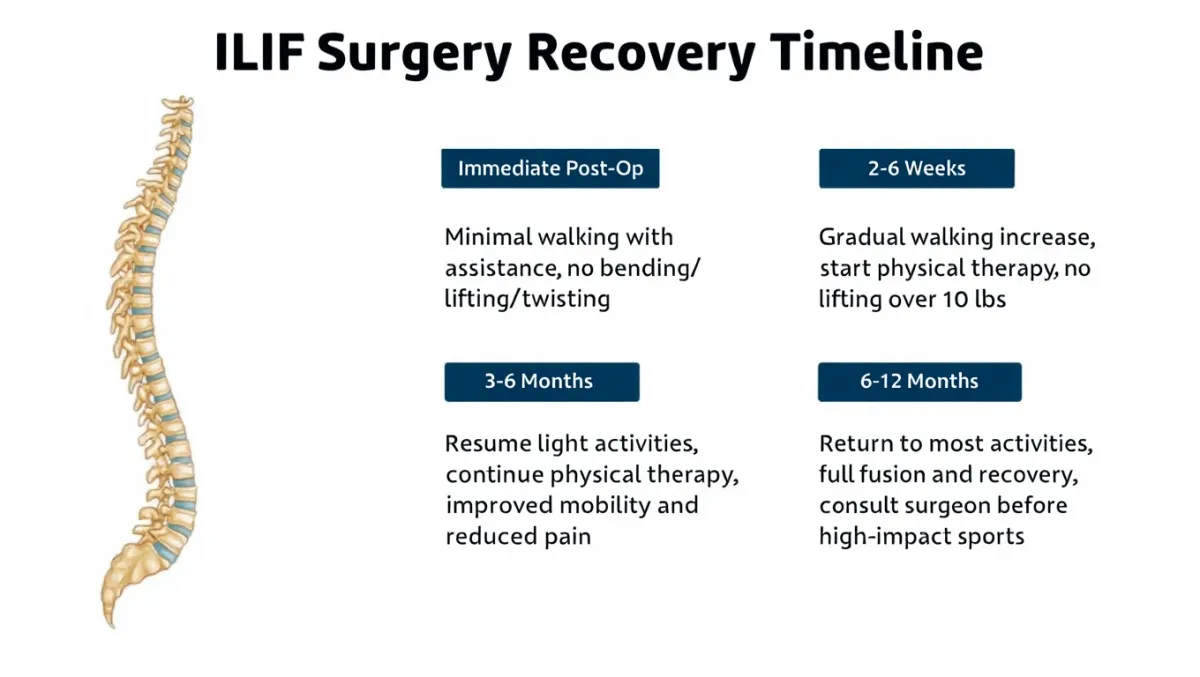
Recovery & Restrictions (typical)
Hospital: Same day or 1 night for many MIS cases
0–2 weeks: Walk frequently; protect the back (no bend/lift/twist)
2–6 weeks: Desk work for many; begin guided PT as ordered
6–12 weeks: Build activity; light strength training; follow-up imaging
3–6 months: Most daily activities restored; sport/work restrictions loosen as fusion consolidates
6–12+ months: Fusion maturation; resume strenuous activities as cleared
Pain control: Multimodal plan to limit opioids.
Bracing: Short-term in select patients—see Bracing.
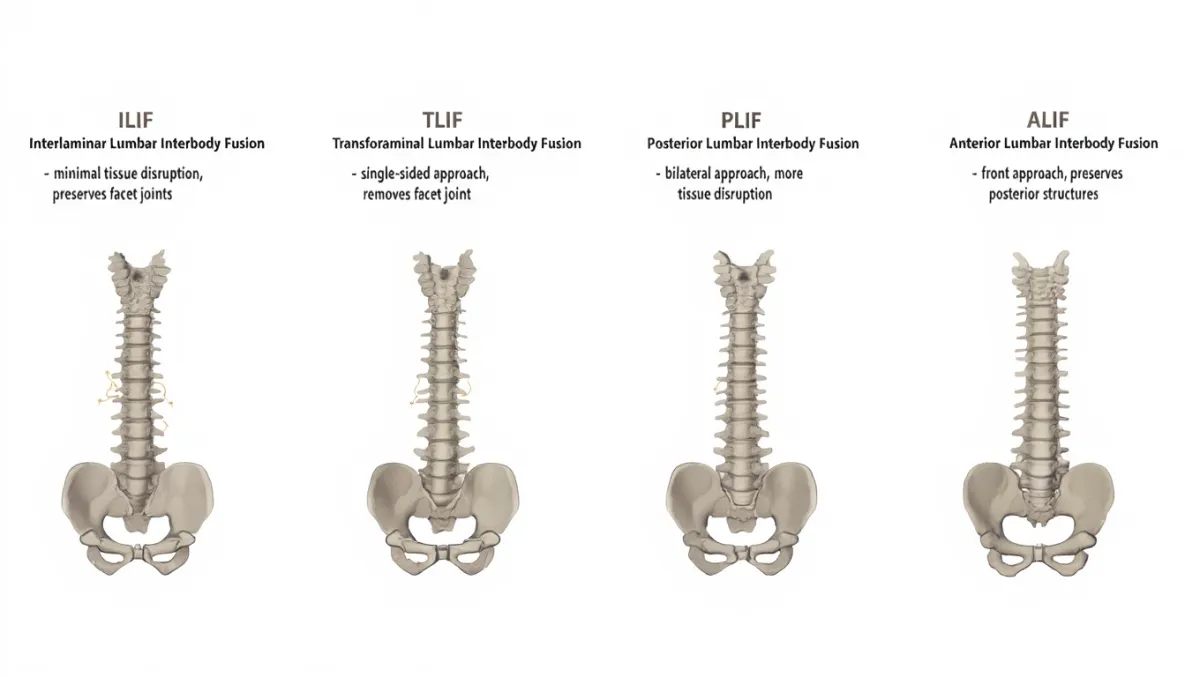
How ILIF Compares (quick context)
vs. XLIF: ILIF is posterior with direct nerve decompression; XLIF is lateral with indirect decompression and less back-muscle manipulation.
vs. MIS TLIF: Very similar goals; ILIF emphasizes the interlaminar window and can be tailored to anatomy and pathology.
Preparing for Surgery
Stop nicotine; optimize diabetes and bone health
Set up home safety (firm chair, no trip hazards, help the first few days)
Follow medication timing (e.g., stop blood thinners per instructions)
Pre-op wash/fasting instructions; bring imaging and med list
Why Desert Spine and Pain
Neurosurgeon-led MIS expertise for both posterior and lateral interbody fusions
Conservative-first, precision surgery when it’s the right move
Clear education, coordinated Physical Therapy, and attentive follow-up
Frequently Asked Questions
Is ILIF the same as TLIF?
They’re closely related MIS posterior fusions. ILIF highlights the interlaminar corridor; TLIF typically includes transforaminal access. Both decompress nerves and insert an interbody cage.
Will I need screws and rods?
Yes, most ILIF cases use percutaneous pedicle screws for stability and to help the fusion heal predictably.
How soon can I return to work?
Desk work often 2–4 weeks. Heavier jobs take longer—we’ll tailor restrictions to your role.
Do I need a brace?
Sometimes short-term. Our goal is to wean as your strength and control improve.
What if I have severe stenosis?
ILIF allows direct decompression, which is ideal for tight stenosis and nerve root crowding.




Dr. David L. Greenwald, MD
Neuro-Spine Surgeon

Call Now!
Desert Spine and Pain
A Spine Specialist is standing by.
Relief is just a phone call away!
Available Around the Clock.
Phone: (602) 566-9500
Email: [email protected]
Contact Us

Schedule a Spine Consultation
If you’re struggling with persistent lower back or leg pain, Interlaminar Lumbar Interbody Fusion (ILIF) may offer the lasting relief you need. Dr. Greenwald and his caring team will perform a comprehensive evaluation to determine whether ILIF is the best option for your condition and guide you through every step of the process. Every step you take toward treatment brings you closer to comfort, stability, and freedom of movement. Schedule your consultation today and learn how Dr. Greenwald’s minimally invasive expertise can help you restore your spine health and quality of life.

Voted Best Spine Doctor
Over 30 Years Experience in Orthopedic & Neuro Spine Surgeries.

Dr. David L. Greenwald, M.D., F.A.C.S.
Neurosurgeon | Spine Surgeon | Regenerative Medicine
Dr. David L. Greenwald, MD, FACS, is a board-certified spine surgeon specializing in Interlaminar Lumbar Interbody Fusion (ILIF), a minimally invasive procedure designed to stabilize the spine and relieve pressure on compressed nerves in the lower back. ILIF is often used to treat degenerative disc disease, spondylolisthesis, and spinal stenosis while preserving more of the natural anatomy compared to traditional fusion techniques. Dr. Greenwald uses advanced imaging and surgical precision to access the spine through a small incision, minimizing tissue disruption and promoting faster recovery. His expertise and patient-centered care have helped individuals throughout South Florida regain mobility, reduce pain, and return to an active lifestyle with improved spinal stability.
Book your Spine Care Consultation Today!


Desert Spine and Pain
Patient Centered & Partner Focused
Quick Links
Resources
Connect With Us
© Desert Spine and Pain. 2026. All Rights Reserved. Sitemap