Back Pain
Lower Back Pain
Relief for Lower Back Pain in Phoenix, AZ
Lower back pain is one of the most common reasons people miss work, skip family activities, or avoid exercise. It can feel scary—especially if you’re not sure what’s wrong or whether you’ll need surgery. At Desert Spine and Pain, we meet you with clarity and compassion. Led by Dr. David L. Greenwald, M.D., FAANS, FACS—a nationally recognized neurosurgeon—we focus on accurate diagnosis, conservative treatments first, and minimally invasive options only when they’re truly necessary. If you’re just starting your research, our overview on Back Pain Conditions explains common causes and pathways to relief. On this page, we’ll go deep on lower back pain: what it is, why it happens, how we find the root cause, and the treatments that help you get your life back.

Over 100 5-Star Reviews!

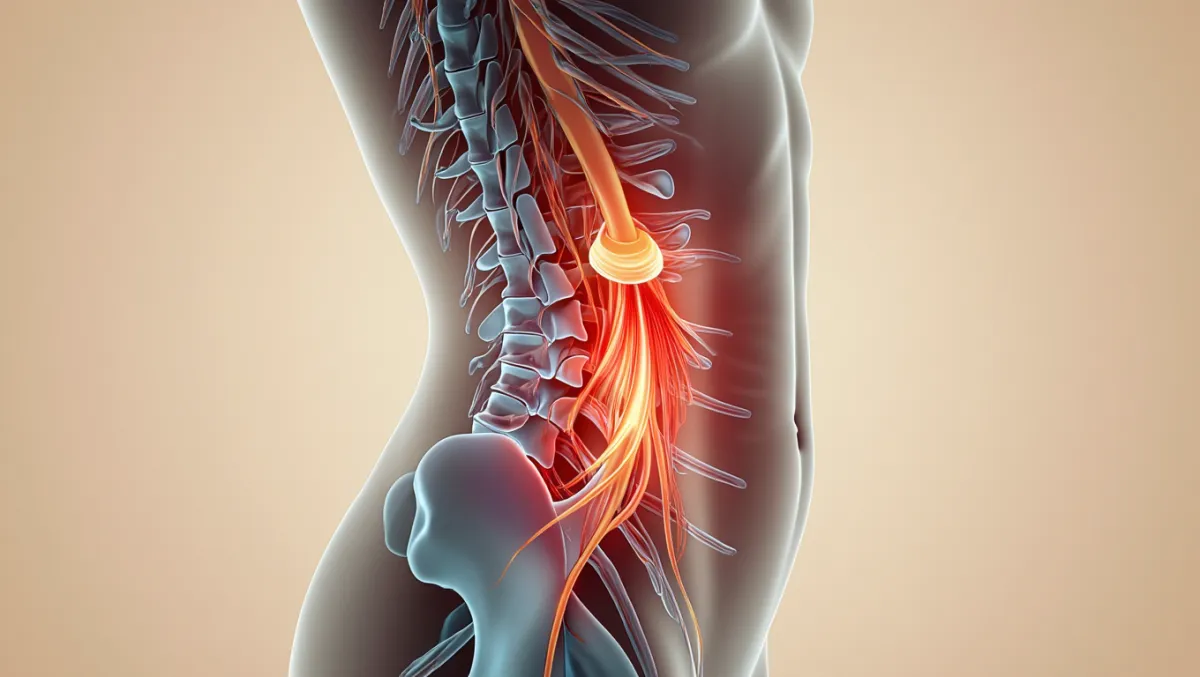
What is Lower Back Pain?
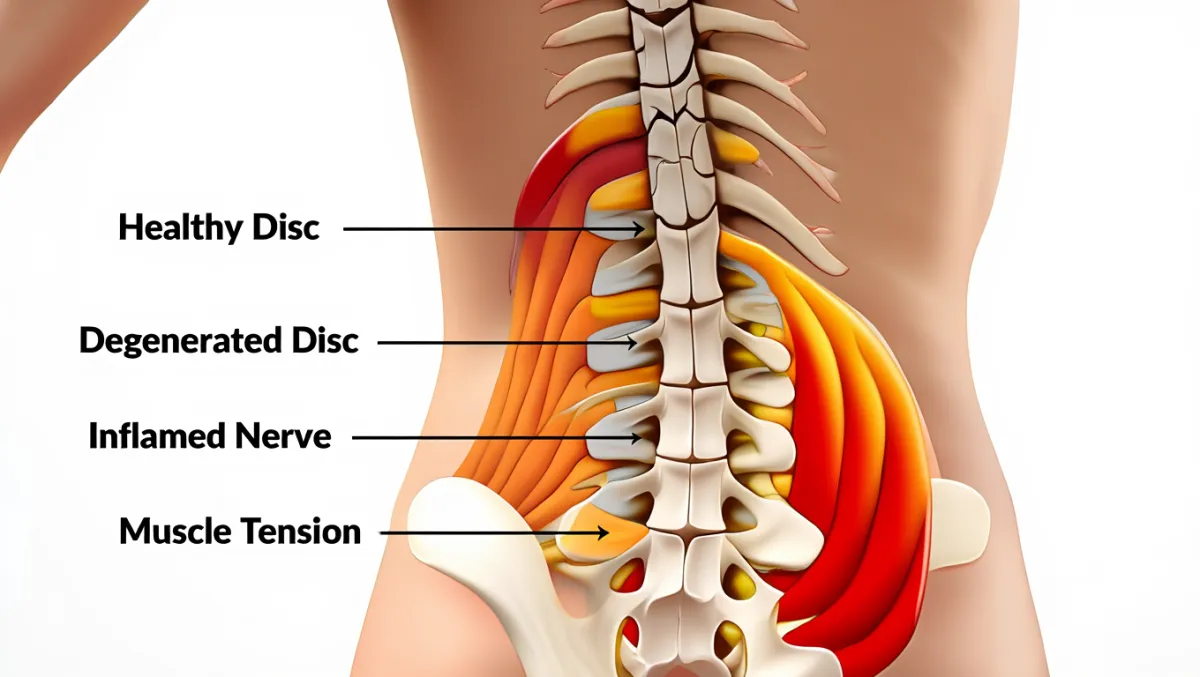
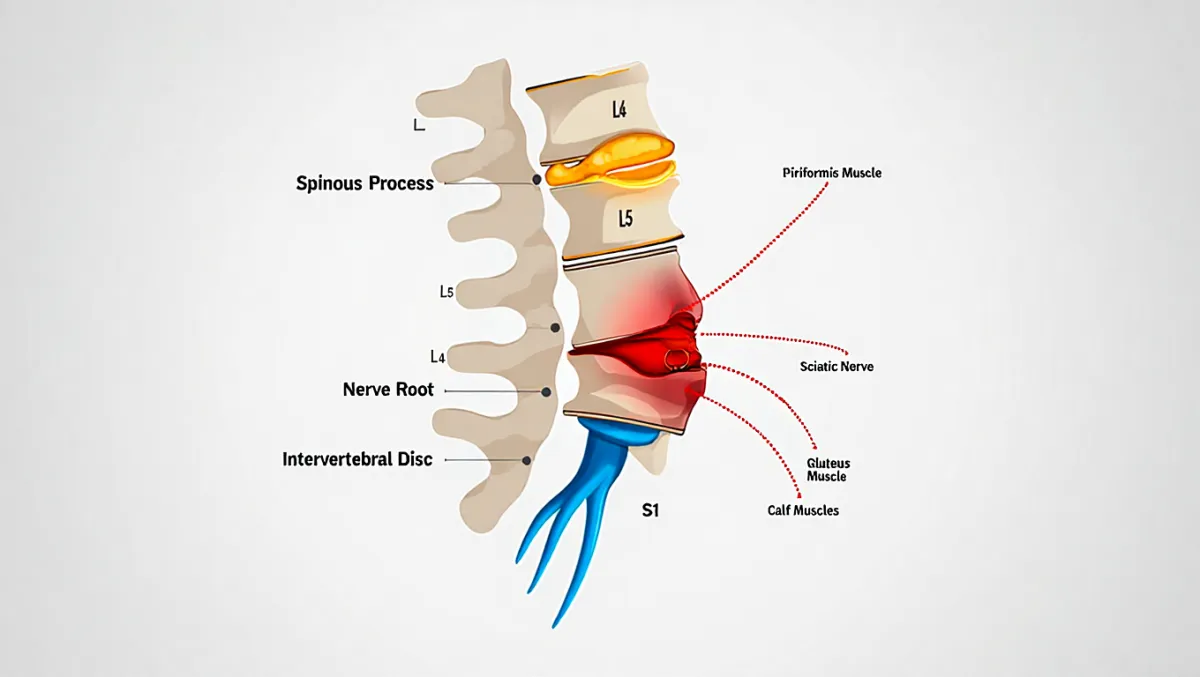
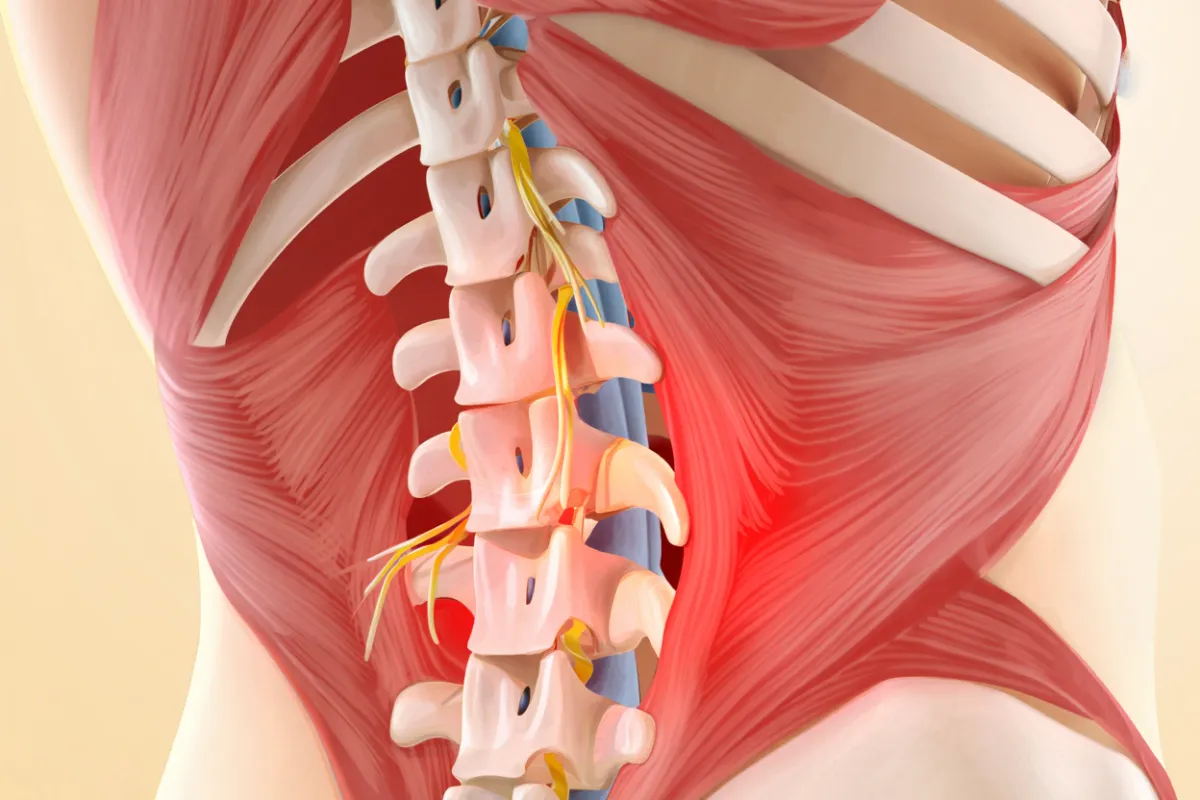
“Lower back pain” describes discomfort arising from structures in the lumbar spine—muscles, ligaments, facet joints, intervertebral disks, nerves, or the vertebral bones themselves. It can be acute (lasting days to weeks) or chronic (lasting 3+ months), and it may be localized or radiate into the buttock or leg depending on which tissues are involved.
Common sources include a simple muscle strain like Lumbar Strain, arthritic facet joints, age-related disk changes, a Herniated Disk, or Spinal Stenosis.
Symptoms
Lower back pain symptoms vary widely. You might notice:
Achy, sharp, or burning pain in the low back
Stiffness, especially in the morning or after sitting
Pain that worsens with bending, lifting, or twisting
Pain that improves with gentle movement or lying down
Buttock or leg pain (sciatica-type symptoms) if a nerve is irritated
Numbness, tingling, or weakness (seek medical care promptly if present)
Red flags—call right away: fever with back pain, recent major trauma, progressive leg weakness, or new bowel/bladder changes.
Why Lower Back Pain Happens (Common Causes)
Muscle or ligament injury (often called “pulled back”): sudden lift, awkward twist, or overuse
Degenerative changes in disks and joints with age
Facet joint arthritis causing localized aching and stiffness
Disk problems, including a bulge or herniation pressing on a nerve
Spinal stenosis (narrowing around nerves)
Sacroiliac (SI) joint irritation—pain where the spine meets the pelvis
Compression fracture in weakened bone (e.g., osteoporosis)
Less common causes include inflammatory conditions, infection, or tumors
If your pain keeps coming back, it’s vital to identify the true pain generator—that’s where our diagnostic process shines.
Our Diagnostic Process (What to Expect)
Conversation & Exam
We’ll listen to your story—when pain started, what worsens/improves it—and perform a focused physical and neurological exam.Imaging (only when needed)
X-ray to review alignment and bone health
MRI to assess disks, nerves, and soft tissues
CT in select cases (e.g., prior surgery, fractures)
Targeted Testing
If the source is still unclear, we may recommend diagnostic blocks (e.g., facet or SI joint) to confirm where pain originates.
Our goal is precision—so your treatment plan addresses the real problem, not just the symptom.
Treatment Options (Conservative First)
Most patients improve without surgery. Your plan is personalized but may include:
Core Conservative Care
Activity modification (brief relative rest, then gentle return to movement)
Medications (short-term anti-inflammatories or muscle relaxants)
Guided Physical Therapy focused on mobility, hip/hamstring flexibility, and core strength
Ergonomics & posture coaching (workstation, lifting mechanics, sleep positions)
Heat/ice for symptom relief
Interventional Pain Options
Epidural Steroid Injections when a disk or stenosis inflames a nerve
Facet, SI joint, or trigger-point injections when appropriate
When Surgery Helps
If significant nerve compression persists or disabling pain does not respond to conservative care, we discuss minimally invasive options tailored to your diagnosis:
Minimally Invasive Surgery (MIS)—tiny incisions, less muscle disruption, faster recovery
Microdiscectomy—removes the fragment pressing on a nerve (excellent for leg-dominant pain from a herniated disk)
Lumbar Fusion—for select cases of instability, deformity, or recurrent problems
We’ll walk you through risks, benefits, expected outcomes, and alternatives so you can make a confident decision.
Timeline, Recovery & Return to Activity
Acute strain: many feel better within 2–6 weeks with self-care and PT
Injection-aided recovery: relief may be rapid (days to weeks), allowing therapy to progress
After MIS microdiscectomy: many resume light activity in 1–2 weeks; full activity often by 6–12 weeks
After lumbar fusion: activity ramps more gradually; bone healing continues for several months
Every recovery is unique—we’ll tailor milestones and check-ins to your goals and lifestyle.
Preparing for Your Visit
Bring prior imaging and a list of treatments you’ve tried
Note where pain travels (does it go past the knee?) and what aggravates/relieves it
Wear comfortable clothing for exam and movement testing
Bring your questions—we’ll answer all of them
At Desert Spine and Pain, there’s no pressure—only honest guidance and premier neurosurgical expertise when you need it.
When Lower Back Pain Is Something Else
Lower back pain can mimic or overlap with other conditions. If your symptoms include radiating leg pain, numbness, or weakness, you may benefit from our pages on Herniated Disk or Spinal Stenosis. If your pain is more localized and achy with morning stiffness, review Lumbar Strain.
Why Choose Desert Spine and Pain?
Premier Phoenix spine center led by Dr. David Greenwald, a board-certified neurosurgeon recognized nationally for complex and minimally invasive spine care
Conservative-first philosophy—surgery only when it’s the best option
Precision diagnosis to target the real cause of pain
Calm, clear communication—we make a scary topic manageable, step by step
Frequently Asked Questions
How do I know if my lower back pain is serious?
Seek care urgently for fever, recent major trauma, progressive leg weakness, or new bowel/bladder changes. Otherwise, schedule an evaluation if pain lasts more than a couple of weeks or interferes with life.
Will I need an MRI right away?
Not always. For many acute cases, exam-guided care comes first. If pain persists, radiates, or includes neurologic symptoms, MRI helps pinpoint the cause.
Do most people with lower back pain need surgery?
No. Most improve with conservative care (PT, medications, injections). Surgery is reserved for persistent, disabling pain or significant nerve compression.
What’s the difference between a strain and a herniated disk?
Strain affects muscles/ligaments (usually localized ache). A herniated disk can press on a nerve, often causing leg pain, numbness, or weakness. See Herniated Disk for details.
If I need surgery, how “minimally invasive” is it?
Many procedures are performed through small incisions with specialized tools. Explore MIS and Microdiscectomy to see what recovery looks like.
Can I prevent future episodes?
Yes—stay active, strengthen your core and hips, optimize posture/ergonomics, and learn safe lifting mechanics. We’ll give you a personalized plan.




Dr. David L. Greenwald, MD
Neuro-Spine Surgeon

Call Now!
Desert Spine and Pain
A Spine Specialist is standing by.
Relief is just a phone call away!
Available Around the Clock.
Phone: (602) 566-9500
Email: [email protected]
Contact Us

Schedule a Consultation Today.
Every step you take toward lasting relief from lower back pain is a step toward reclaiming your comfort and mobility. Dr. David Greenwald and his dedicated team are here to guide you through every stage of your recovery with expert care and compassion. Whether your pain is new or chronic, we’ll work with you to find the right solution—so you can move, work, and live without constant discomfort. You deserve to feel your best, and we’re here to make it happen. Schedule your consultation today and take the first step toward a pain-free future.

Voted Best Back Doctor
Over 30 Years Experience in Orthopedic & Neuro Spine Surgeries.

Dr. David L. Greenwald, M.D., F.A.C.S.
Neurosurgeon | Spine Surgeon | Regenerative Medicine
Dr. David L. Greenwald, MD, FACS, is a board-certified spine surgeon specializing in the diagnosis and treatment of lower back pain caused by conditions such as degenerative disc disease, herniated discs, spinal stenosis, and other spinal disorders. With decades of experience in minimally invasive spine surgery, Dr. Greenwald focuses on providing lasting relief while preserving mobility and function. He takes a personalized approach to care—starting with a thorough evaluation, advanced imaging, and conservative treatment when appropriate, before recommending surgical options only when necessary. Patients throughout South Florida trust Dr. Greenwald for his expertise, precision, and compassionate approach to restoring spine health and improving quality of life.
Book your Spine Care Consultation Today!


Desert Spine and Pain
Patient Centered & Partner Focused
Quick Links
Resources
Connect With Us
© Desert Spine and Pain. 2026. All Rights Reserved. Sitemap