Decompression
Ulnar Nerve Decompression
Relieving Pressure at the “Funny Bone” Nerve
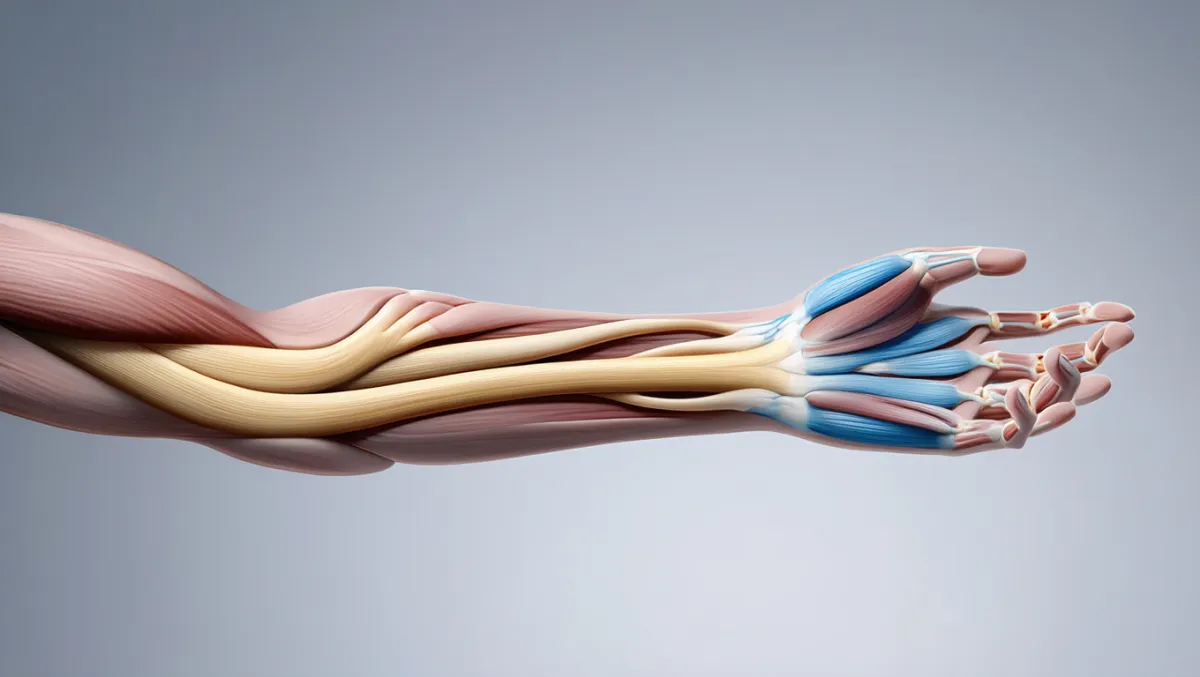
The ulnar nerve runs from the neck through the arm to the hand, passing through narrow tunnels at the elbow (cubital tunnel) and wrist (Guyon’s canal). Compression at these sites can cause numbness, tingling, pain, or weakness in the hand and forearm. This condition is often called cubital tunnel syndrome. At Desert Spine and Pain, neurosurgeon Dr. David L. Greenwald, M.D., FAANS, FACS offers ulnar nerve decompression surgery for patients who don’t improve with bracing, activity changes, or injections. Using minimally invasive and microsurgical techniques, we relieve nerve pressure to restore function and prevent permanent damage.

Over 100 5-Star Reviews!

What Is Ulnar Nerve Decompression?
In simple terms: The surgery creates more room for the ulnar nerve at the elbow (or wrist) by removing tight structures pressing on it.
Scientifically: Ulnar nerve decompression involves release of fascial bands, Osborne’s ligament, and flexor carpi ulnaris aponeurosis, with or without anterior transposition. The goal is to relieve chronic nerve entrapment and restore conduction.
Conditions Treated
Cubital tunnel syndrome (ulnar nerve compression at the elbow)
Guyon’s canal syndrome (ulnar nerve compression at the wrist)
Progressive numbness, tingling, or hand weakness despite conservative care
Muscle wasting in severe cases requiring urgent decompression
Non-Surgical Care (Tried First)
Activity modification (avoiding prolonged elbow flexion or leaning on elbows)
Night splints to keep elbows straight
Anti-inflammatory medications
Physical therapy for stretching and nerve gliding
Corticosteroid injections (select cases)

The Ulnar Nerve Decompression Procedure: Step by Step
Plain-English Overview
Anesthesia: Local anesthesia with sedation or general anesthesia.
Incision: Small incision made along the inside of the elbow.
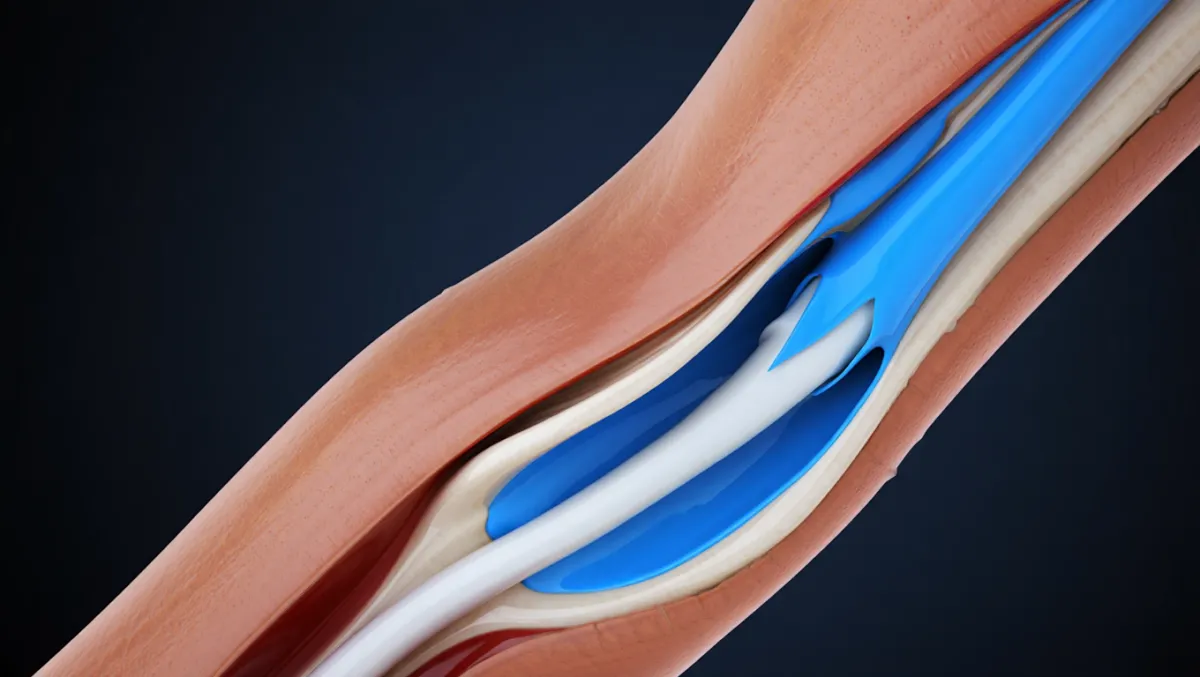
Nerve release: Tight tissue (ligaments and fascia) around the nerve is cut to relieve pressure.
Transposition (if needed): The nerve is moved to a new position in front of the elbow for better protection.
Closure: The incision is closed with sutures; patients often go home the same day.
Surgeon-Level Detail
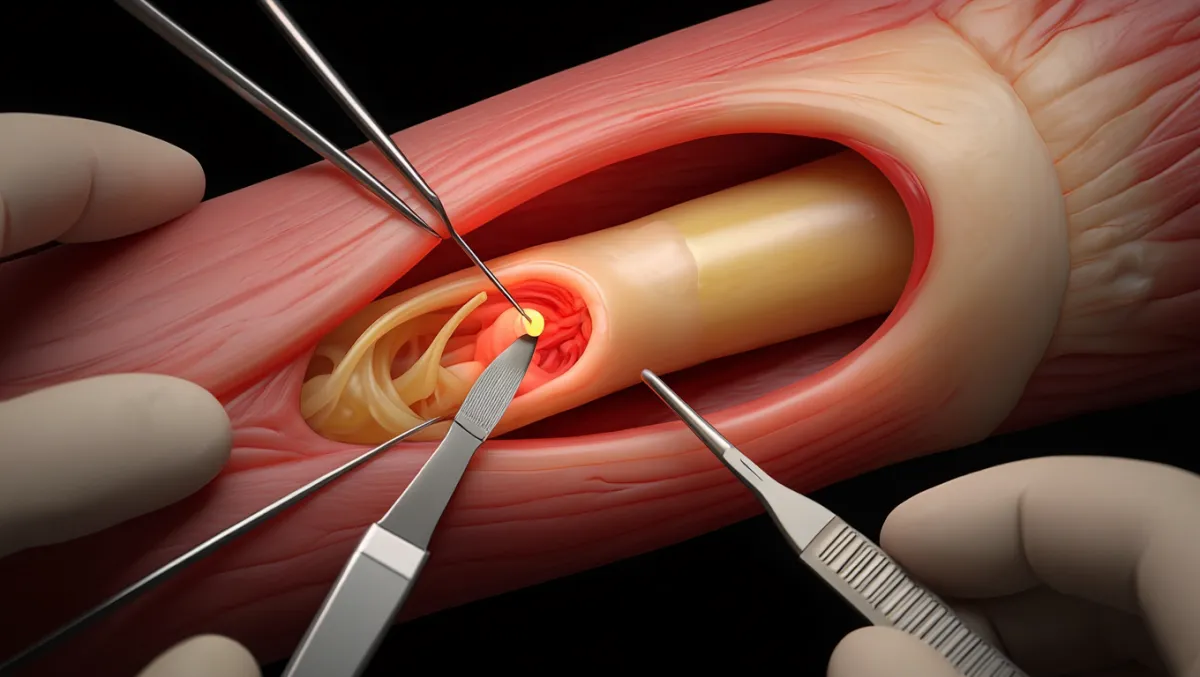
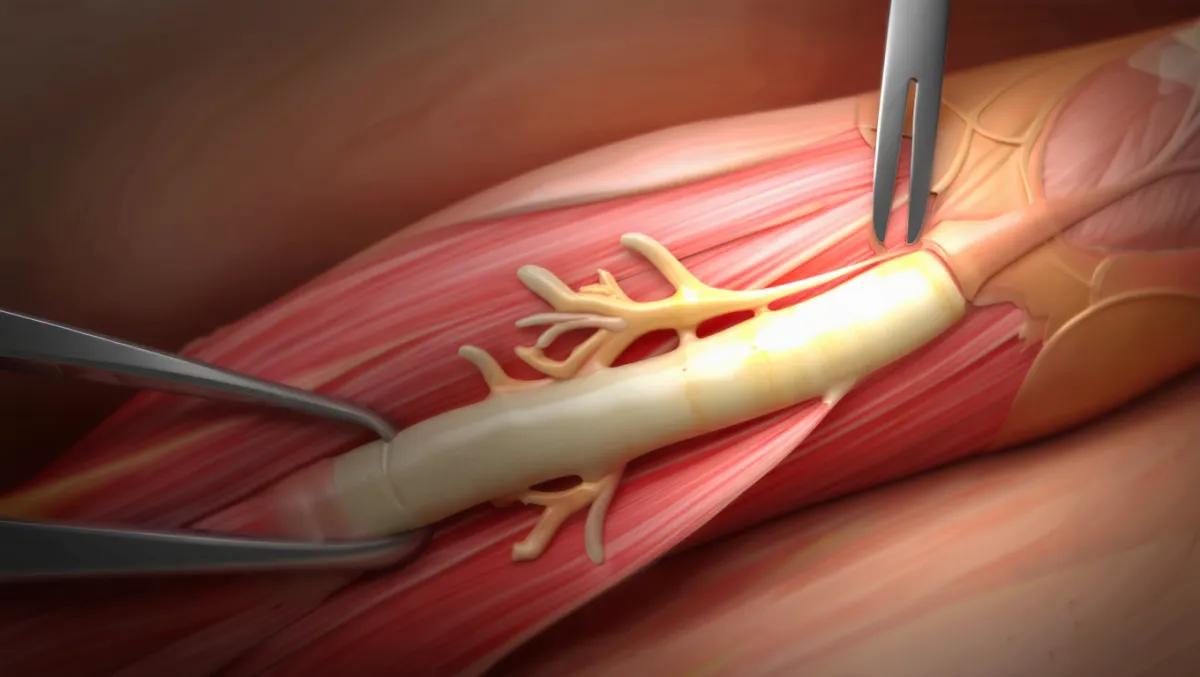
Exposure: Small curvilinear incision along medial elbow; ulnar nerve identified proximally and distally.
Decompression: Osborne’s ligament, FCU aponeurosis, and arcade of Struthers released under loupe/microscope.
Nerve mobilization: Ensure gliding without kinking through elbow ROM.
Transposition (if performed): Nerve moved anteriorly into subcutaneous, intramuscular, or submuscular bed; secured to prevent subluxation.
Closure: Meticulous hemostasis; layered closure; splinting varies by technique.
Benefits of Ulnar Nerve Decompression
Relief of numbness, tingling, and pain
Prevents permanent nerve damage and hand muscle wasting
Outpatient surgery with small incision
Often rapid improvement in night symptoms and grip strength
Risks & Limitations
Infection, bleeding, scar tenderness
Nerve injury (rare with microsurgical technique)
Incomplete relief if nerve already severely damaged
Recurrence possible if scar tissue develops
Recovery may be slower in chronic cases with muscle wasting

Recovery Timeline
Day of surgery: Outpatient procedure; arm in soft dressing
Weeks 1–2: Suture removal; light activity only
Weeks 2–6: Gradual return to daily use; therapy for nerve glides and strength
3–6 months: Ongoing improvement in sensation and strength
6–12 months: Nerve recovery continues; full benefit realized over time
Why Choose Desert Spine and Pain?
Neurosurgical expertise: Dr. Greenwald is highly skilled in precision nerve decompressions
Minimally invasive approach: Small incision, less pain, faster healing
Comprehensive care: From diagnosis with EMG/NCV testing to surgery and rehab
Compassionate focus: We listen, reassure, and guide you through recovery
Frequently Asked Questions
How do I know if I need ulnar nerve surgery?
If symptoms persist despite splints, therapy, and activity changes—or if weakness is worsening—surgery may be needed.
Will surgery restore full sensation and strength?
Relief of tingling is often rapid. Numbness and weakness improve gradually, but recovery depends on how long the nerve has been compressed.
Is ulnar nerve decompression painful?
Discomfort is usually mild and improves within weeks. Most patients are surprised at how manageable recovery is.
What’s the difference between decompression and transposition?
Decompression simply releases pressure. Transposition moves the nerve to a safer location if instability is present.
How does Desert Spine and Pain perform this differently?
We use microsurgical techniques, careful patient selection, and neurosurgical precision to maximize outcomes while minimizing risk.




Dr. David L. Greenwald, MD
Neuro-Spine Surgeon

Call Now!
Desert Spine and Pain
A Spine Specialist is standing by.
Relief is just a phone call away!
Available Around the Clock.
Phone: (602) 566-9500
Email: [email protected]
Contact Us

Book a Consultation.
If you’re experiencing numbness, tingling, or weakness in your hand or forearm, Ulnar Nerve Decompression may provide the relief you need. Dr. Greenwald and his compassionate team will perform a thorough evaluation, review diagnostic imaging or nerve studies, and recommend the best treatment for your symptoms. Every step you take toward specialized nerve care brings you closer to restored comfort and confidence. Schedule your consultation today and let Dr. Greenwald help you regain strength and mobility in your arm and hand.

Voted Best Spine Doctor
Over 30 Years Experience in Orthopedic & Neuro Spine Surgeries.

Dr. David L. Greenwald, M.D., F.A.C.S.
Neurosurgeon | Spine Surgeon | Regenerative Medicine
Dr. David L. Greenwald, MD, FACS, is a board-certified spine and peripheral nerve surgeon with advanced expertise in Ulnar Nerve Decompression, a surgical procedure that relieves pressure on the ulnar nerve—commonly affected at the elbow in a condition known as cubital tunnel syndrome. This condition can cause numbness, tingling, or weakness in the ring and little fingers, and sometimes result in grip loss or hand dysfunction. Dr. Greenwald uses minimally invasive techniques to release the compressed nerve, restore normal function, and prevent further nerve damage. His precision, experience, and patient-centered approach have helped individuals throughout South Florida regain strength, reduce discomfort, and improve hand and arm mobility.
Book your Spine Care Consultation Today!


Desert Spine and Pain
Patient Centered & Partner Focused
Quick Links
Resources
Connect With Us
© Desert Spine and Pain. 2026. All Rights Reserved. Sitemap
